Confusing Deadly Cancer with Flu Delays Treatment
The prevalence of lymphoma was recently highlighted when former Top Ten tennis player Carla Suarez Navarro withdrew from the US Open following her diagnosis with Hodgkin Lymphoma. Lymphoma is the most common form of blood cancer, with an individual diagnosed every 27 minutes. Over 735,000 people diagnosed with lymphoma, including Chronic Lymphocytic Leukaemia (CLL), every year across the world.
The past few months have been especially challenging for those with lymphoma. Not only have they needed to shield to reduce the risk of Covid-19 exposure, but many treatments have been paused or changed. Furthermore, many clinical trials were also put on hold and are only now beginning to restart, according to Lymphoma Action. During Blood Cancer Awareness Month in September and World Lymphoma Awareness Day on 15th September, the focus is supporting individuals – and their carers - living with blood cancer.
Confusing Symptoms
Lymphoma is the most commonly occurring blood cancer and the third most common childhood cancer. Occurring when abnormal lymphocytes grow out of control and collect in the lymph nodes or other parts of the body, one million people around the world are living with lymphoma today. Yet many people are still unaware of lymphoma and that it is a life-threatening form of cancer.
One of the diagnostic challenges for clinicians is that there are currently no screening tests for lymphomas – indeed, the signs and symptoms of lymphoma can often be mistaken for other less serious illnesses, including flu.
According to the Lymphoma Coalition, many patients delay going to the doctor because they don’t realise they have cancer. A global patient survey revealed that 18% of patients waited six to 12 months to visit a GP after first experiencing symptoms; with 8% waiting up to two years, 5% five years and 4% over five years.
The most common symptom is painless swelling in a lymph node, primarily neck or armpits but also the groin and abdomen. Some patients, however, have no swelling, instead experiencing night sweats, weight loss, chills, a lack of energy, or itching. There is usually no pain involved, especially when the lymphoma is in the early stage of development. However, these symptoms persist over time with lymphoma and cannot be explained by an infection or another disease.
Additional research from Lymphoma Action confirms that 17% of patients were initially treated by a GP for a different condition, 28% were sent for non-urgent referral to a specialist, while 11% were seen as emergency/ A&E patients. Just 7% were sent to hospital for same day treatment – and 38% were referred by the GP under the ‘two week’ wait scheme.
Diagnosing Lymphoma
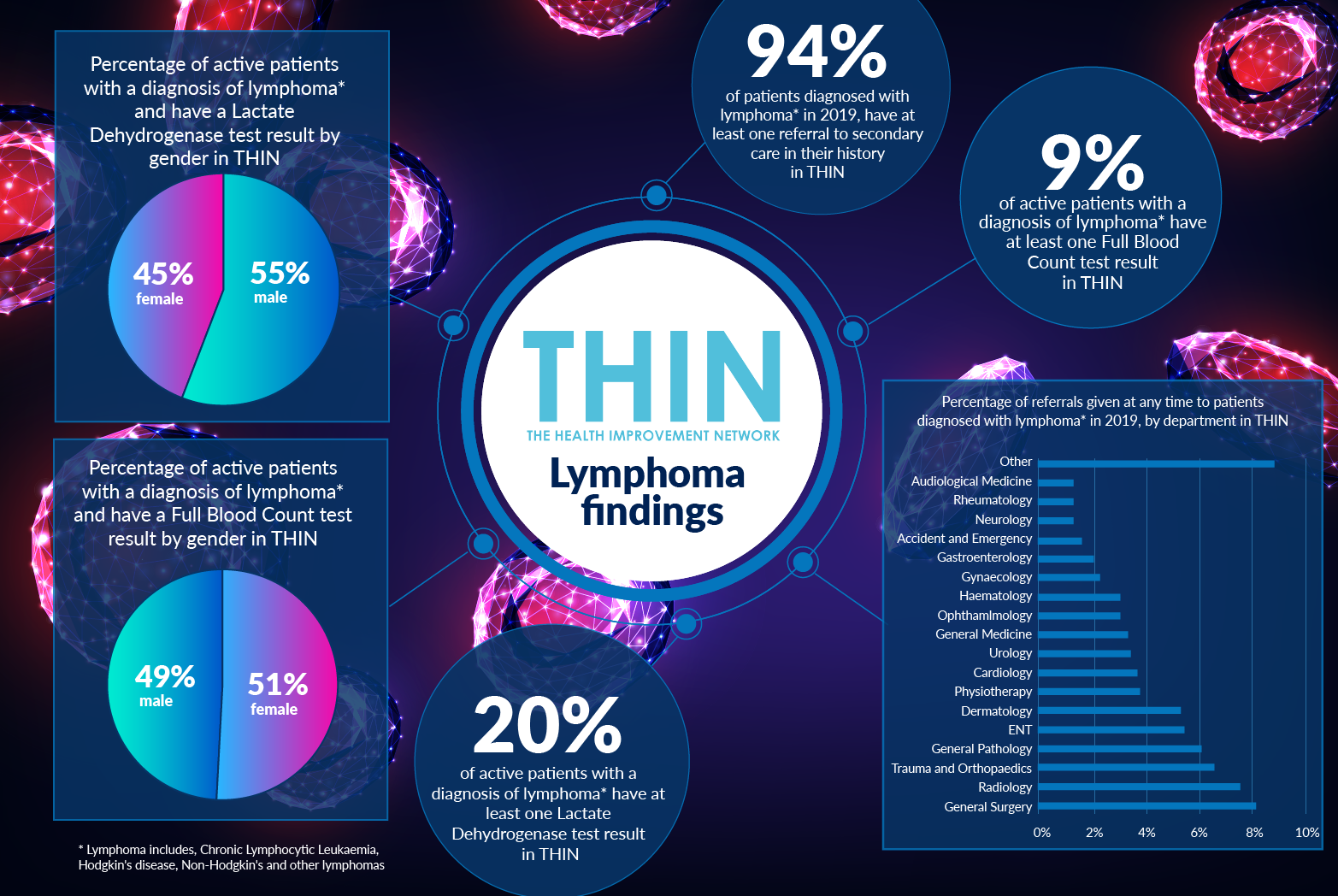
Analysis of The Health Improvement Network (THIN®), a Cegedim Database, underlines the diagnostic challenges associated with lymphoma: 94% of patients diagnosed with lymphoma* in 2019, have at least one referral to secondary care in their history in THIN®.
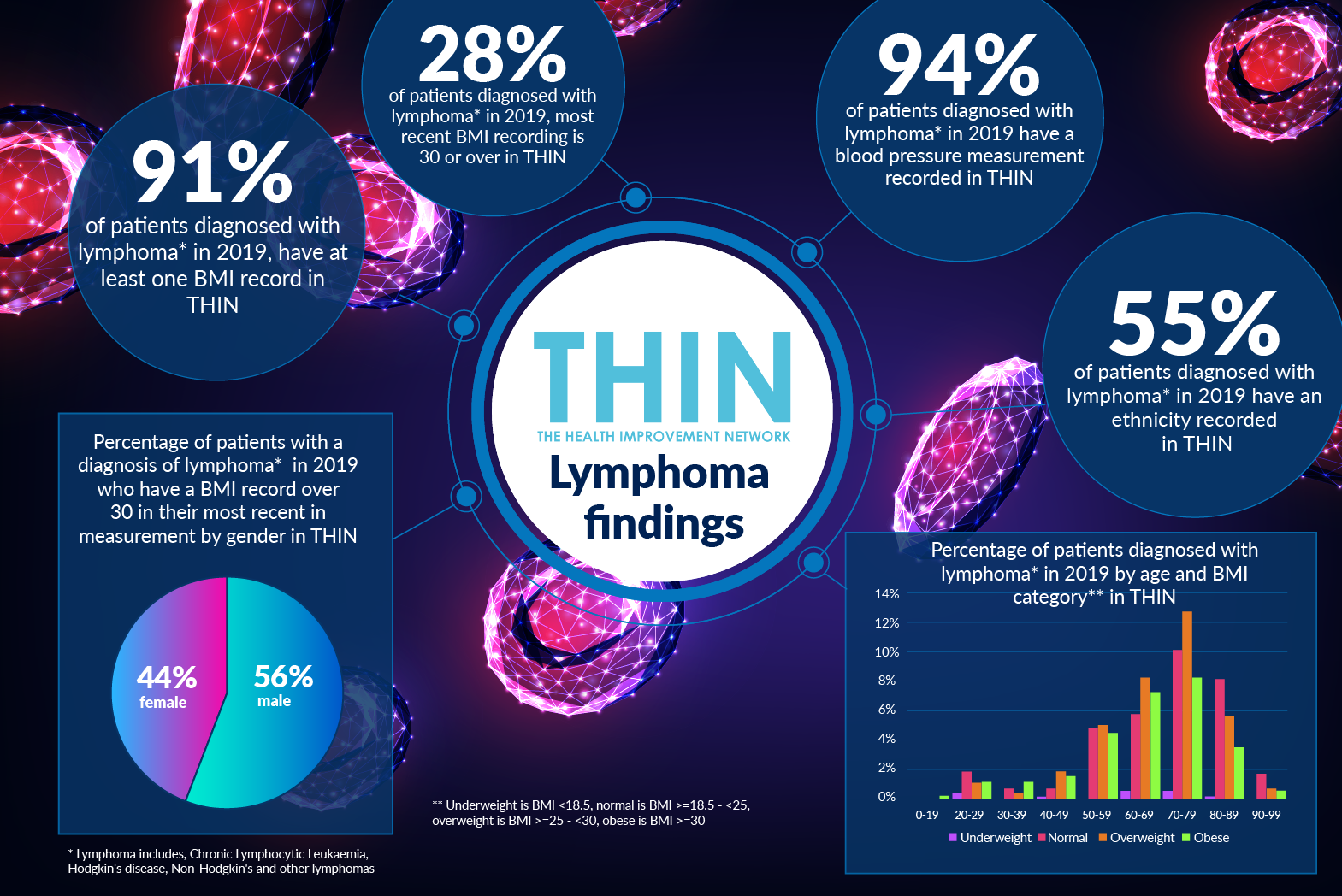
Blood tests play a key role in both identifying lymphoma and tracking a patient’s response to treatment, including chemotherapy, antibody therapy and targeted drugs, all of which can cause low blood counts. Just 9% of active patients with a diagnosis of lymphoma have at least one Full Blood Count test result in THIN®. One fifth (20%) of active patients with a diagnosis of lymphoma have at least one Lactate Dehydrogenase test result, which can reveal inflammation, in THIN®.
Understanding Comorbidities
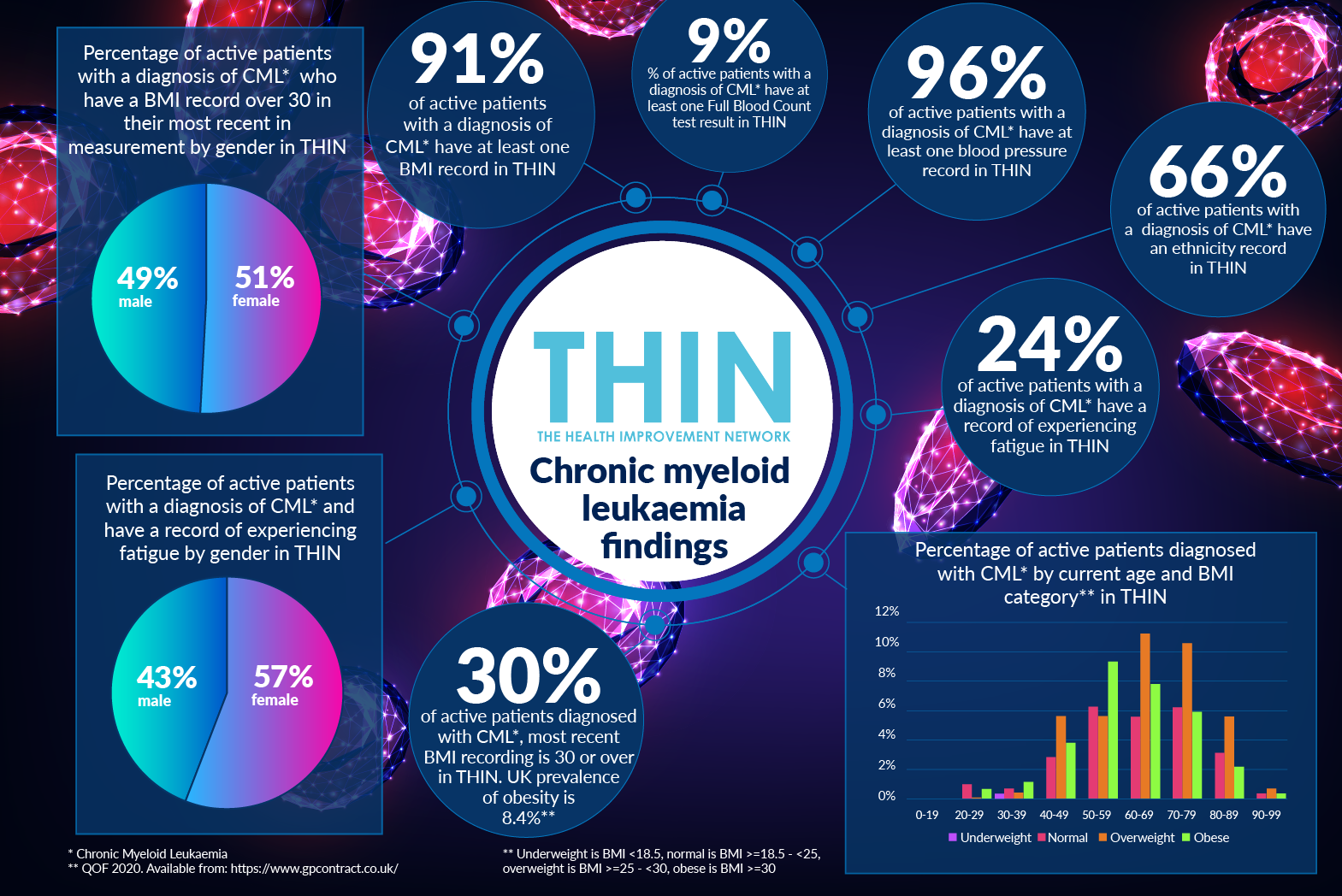
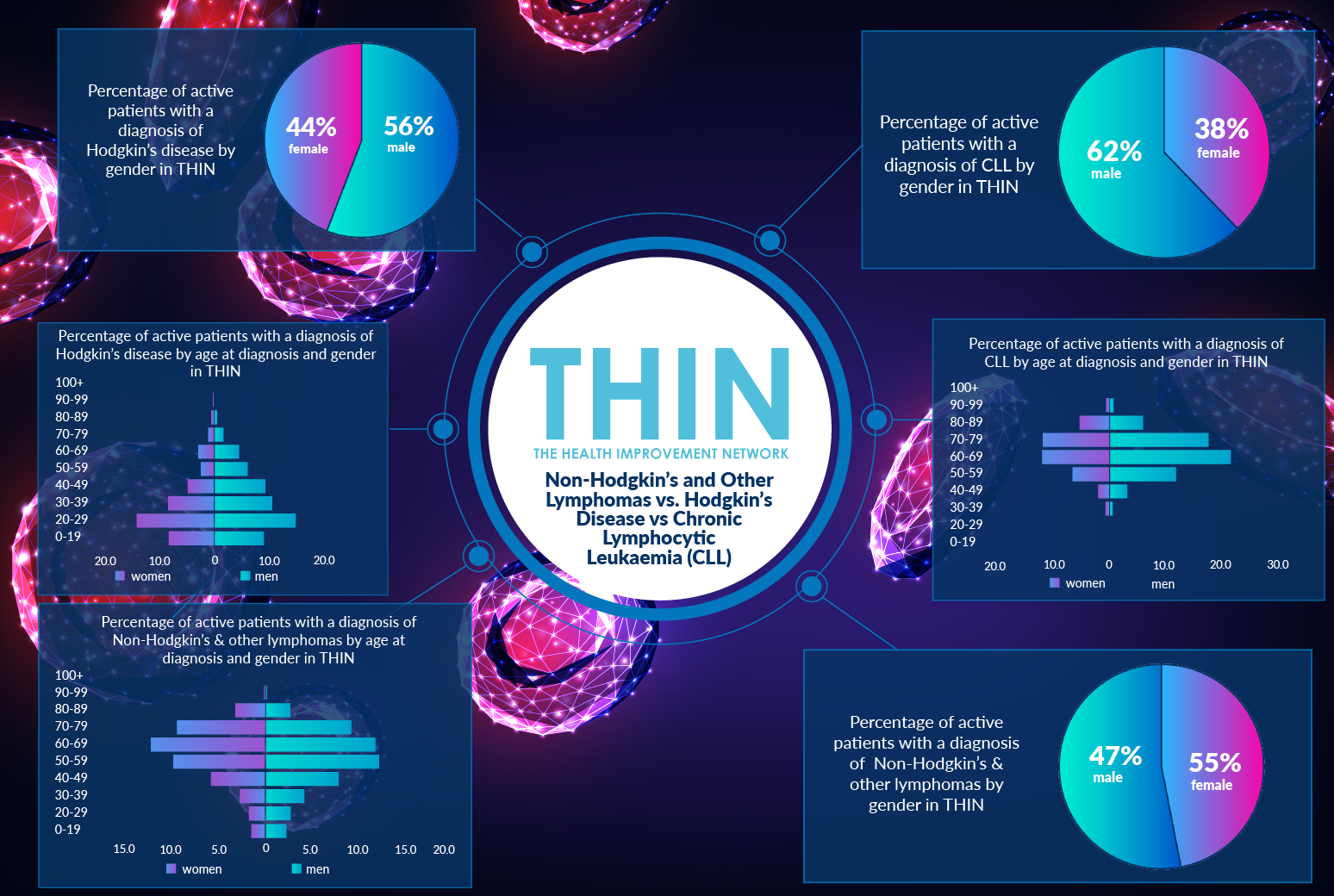
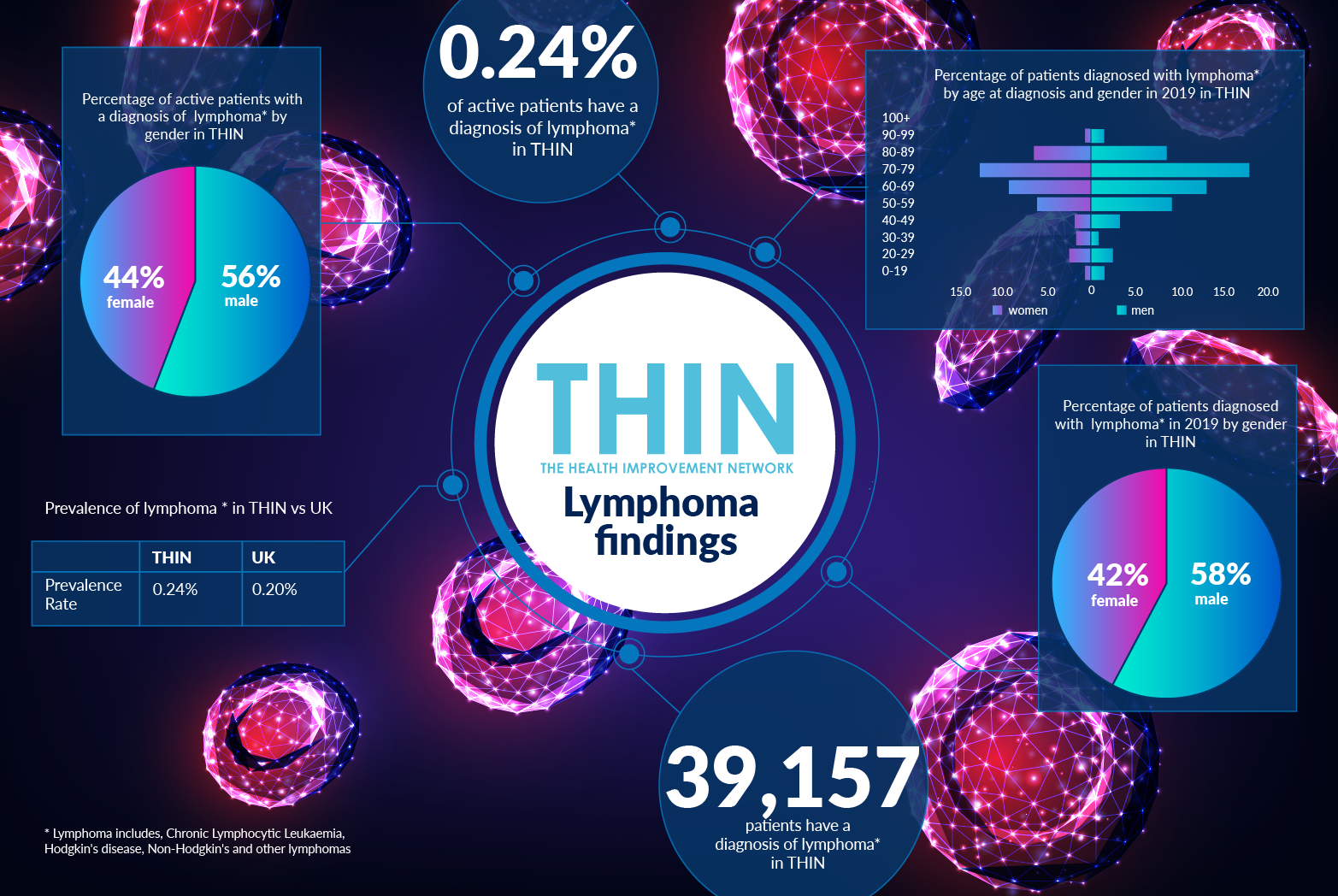
The exact causes and risk factors are still unknown. Research continues around the world, which is why population health data, as provided by THIN®, is vital. With 39,157 patients with a diagnosis of lymphoma within THIN® – representing 0.24% of active patients - our analysis confirms the male bias in lymphoma patients. Within THIN®, men (56%) are more likely to be diagnosed with lymphoma than women (44%). The average age at diagnosis is mid 60s for all patients.
THIN® data also confirms that men are more likely to experience the comorbidities associated within lymphoma. 7% of active patients with a diagnosis of lymphoma also have a diagnosis of COPD in THIN® – 59% are male. 14% of active patients with a diagnosis of lymphoma also have a diagnosis of diabetes in THIN® – 63% are male. 12% of active patients with a diagnosis of lymphoma also have a diagnosis of coronary heart disease in THIN® – 63% are male.
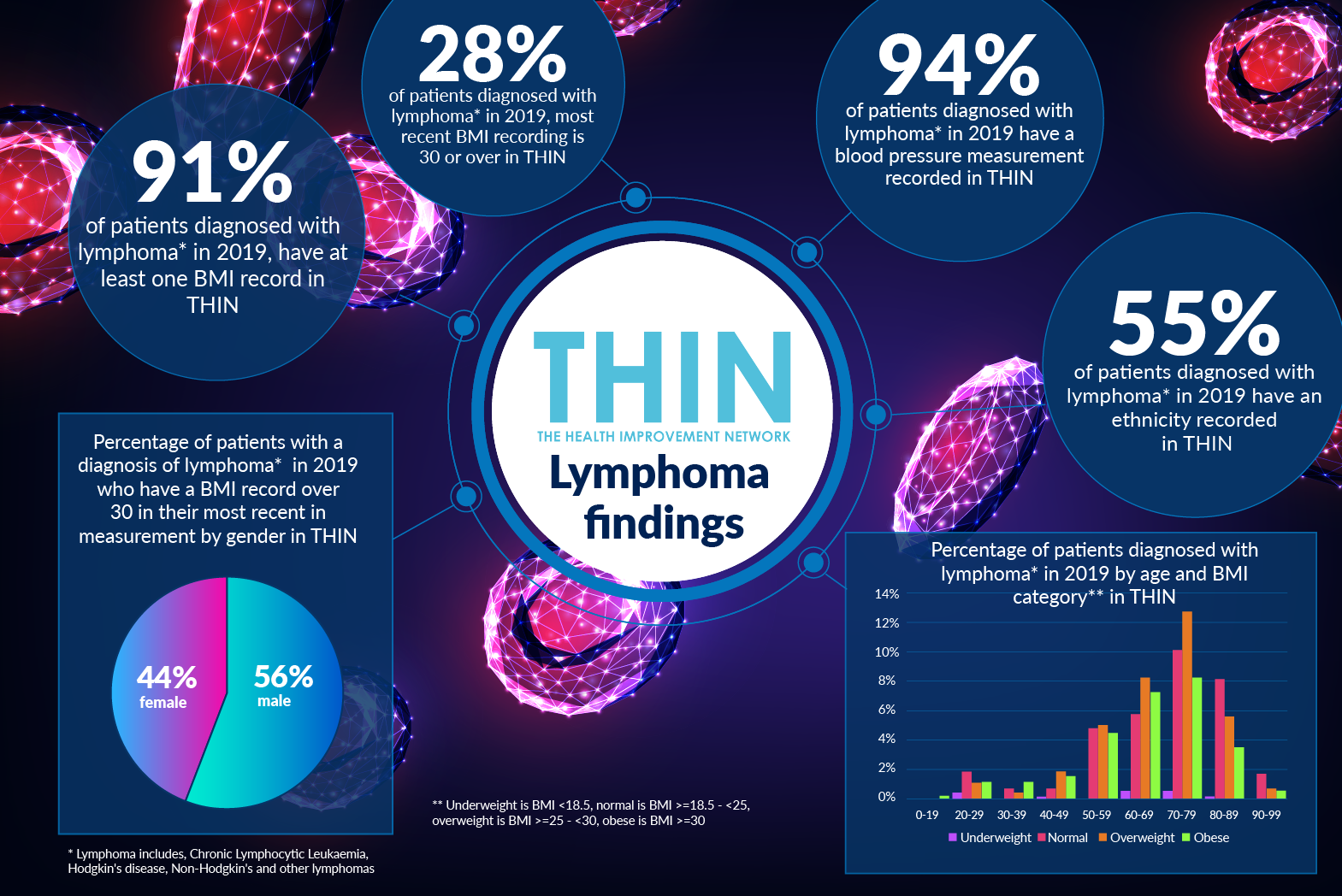
Weight is also a factor. 91% of patients diagnosed with lymphoma in 2019, have at least one BMI record in THIN® – for over a quarter (28%), the most recent BMI recording is 30 or over.
Different Diagnostic Approach
This is a complex cancer, with more than 60 subtypes with varying diagnoses, treatment options and outcomes. Generally categorised either into Hodgkin lymphoma or non-Hodgkin lymphoma, each subtype requires different diagnostic evaluation and treatment protocols and will result in different outcomes.
Some forms are aggressive, others indolent and in most cases, there is no known cause. While understanding is increasing, there remains a disparity between the experiences of lymphoma patients and those of other cancer types, making the traditional cancer service approach of prevention, early detection, speedy treatment and aftercare less effective.
With the well-publicised delays to cancer diagnosis and treatment as a result of Covid-19, clinicians are under significant pressure. With cancers such as lymphoma that can easily be mistaken for other illnesses, the use of epidemiological health data such as THIN® will play an important role in improving understanding. Better insight into comorbidities will help not only with earlier identification and awareness but also getting a patient to the lymphoma specialist able to diagnose the correct subtype of lymphoma to ensure they receive the right treatment at the right time for the right subtype.
*Lymphoma includes, Chronic Lymphocytic Leukemia, Hodgkin's disease, Non-Hodgkin’s and other lymphoma
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.