World Contraception Day
On the 26th September, it is World Contraception Day with the mission to spread the word and raise awareness about contraception and safe sex, enabling young people to make informed choices on their sexual and reproductive health.
Launched in 2007, the aim is to help each new generation of adults make informed decisions so that every pregnancy is a planned one. World Contraception Day is supported by a coalition of 15 international Non-Governmental Organizations (NGOs), governmental organisations and scientific and medical societies with an interest in sexual and reproductive health and is sponsored by Bayer AG.
Contraception Methods – How to Decide?
With so many birth control options available, choosing a most suitable form can be confusing, even discouraging for many young adults. Which method protects against sexually transmitted infections (STIs)? What about convenience of use? How effective are they? What side effects might they have? And the questions are not only for younger people. For older women, other considerations might include concerns over the long-term use of oral contraception.
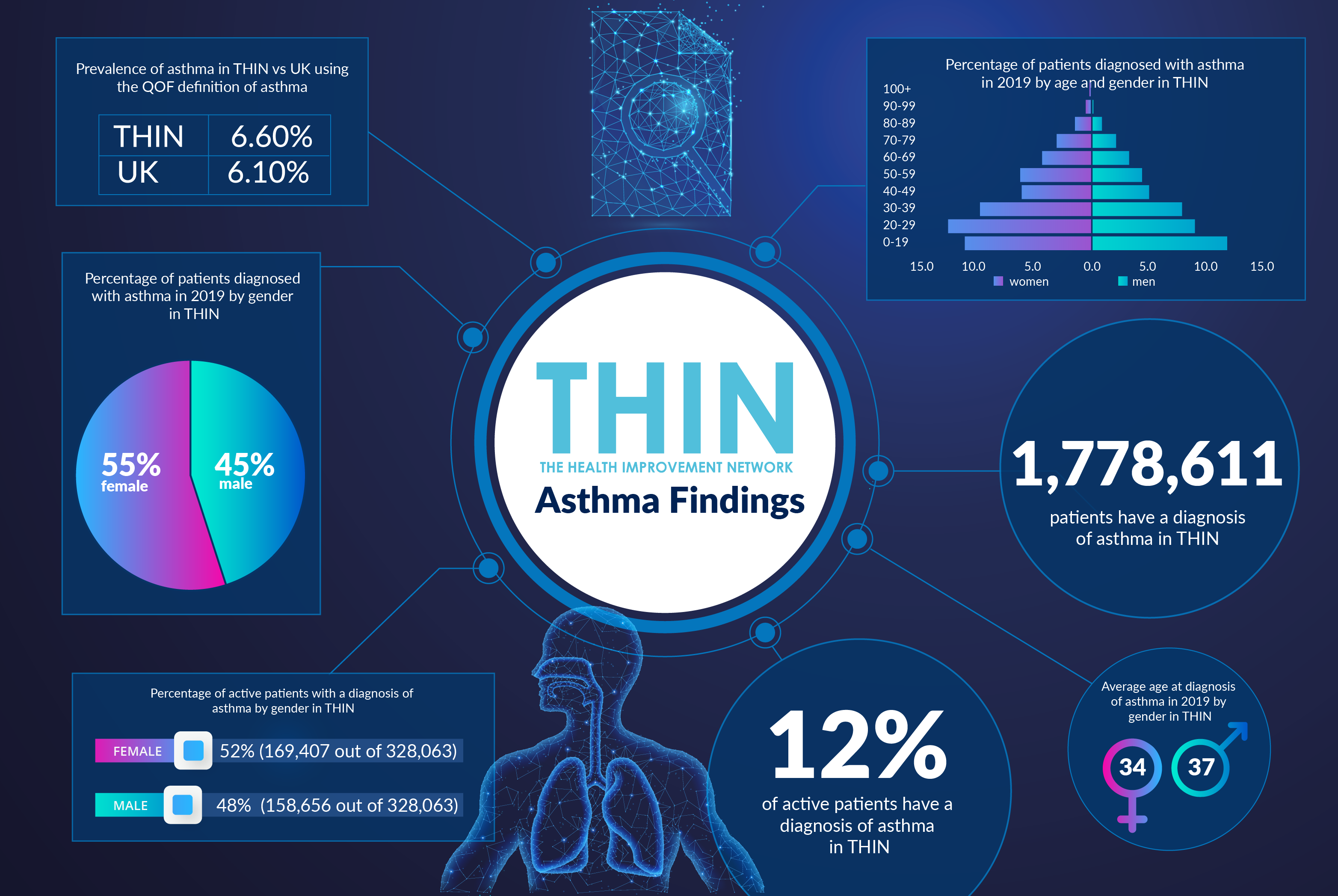
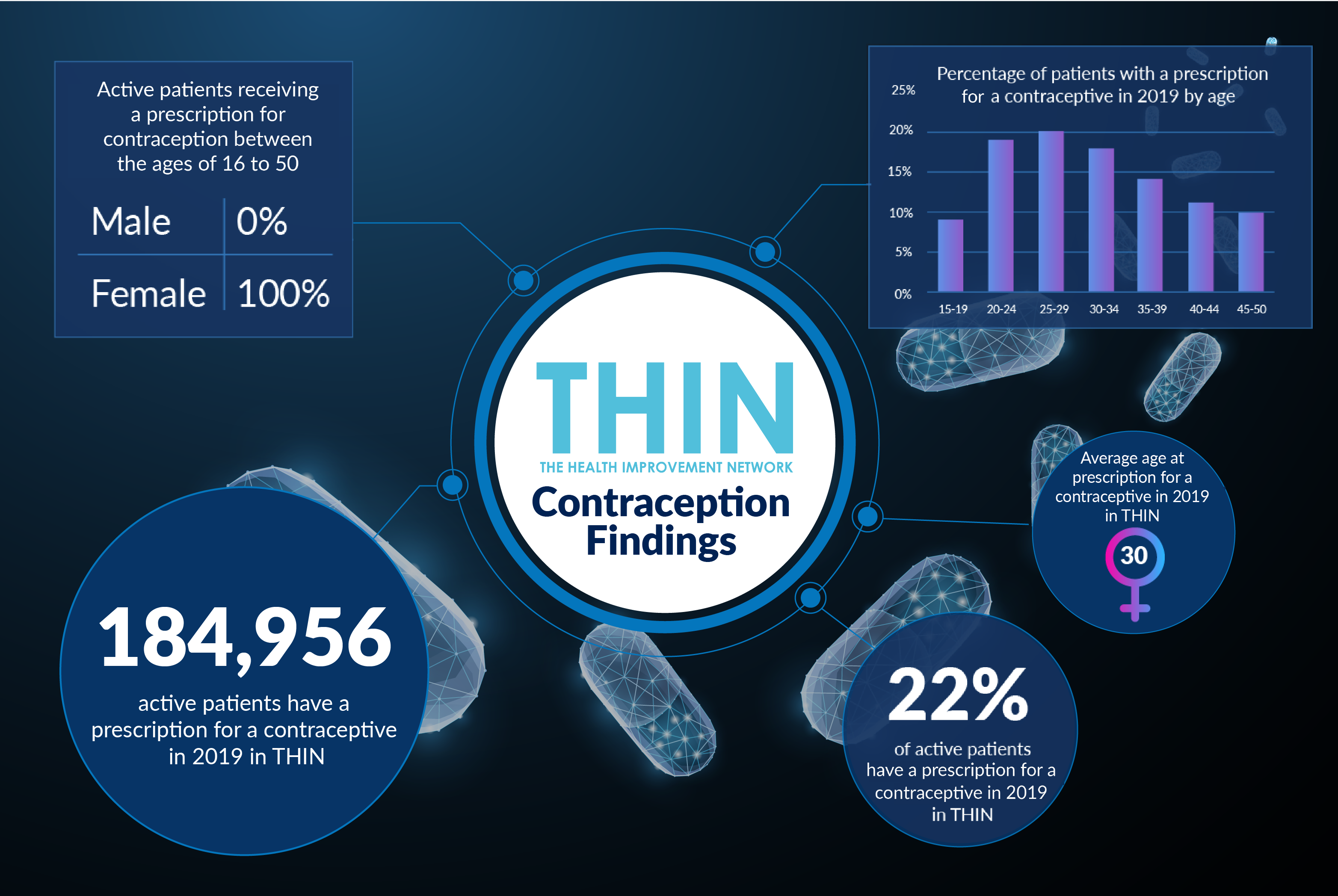
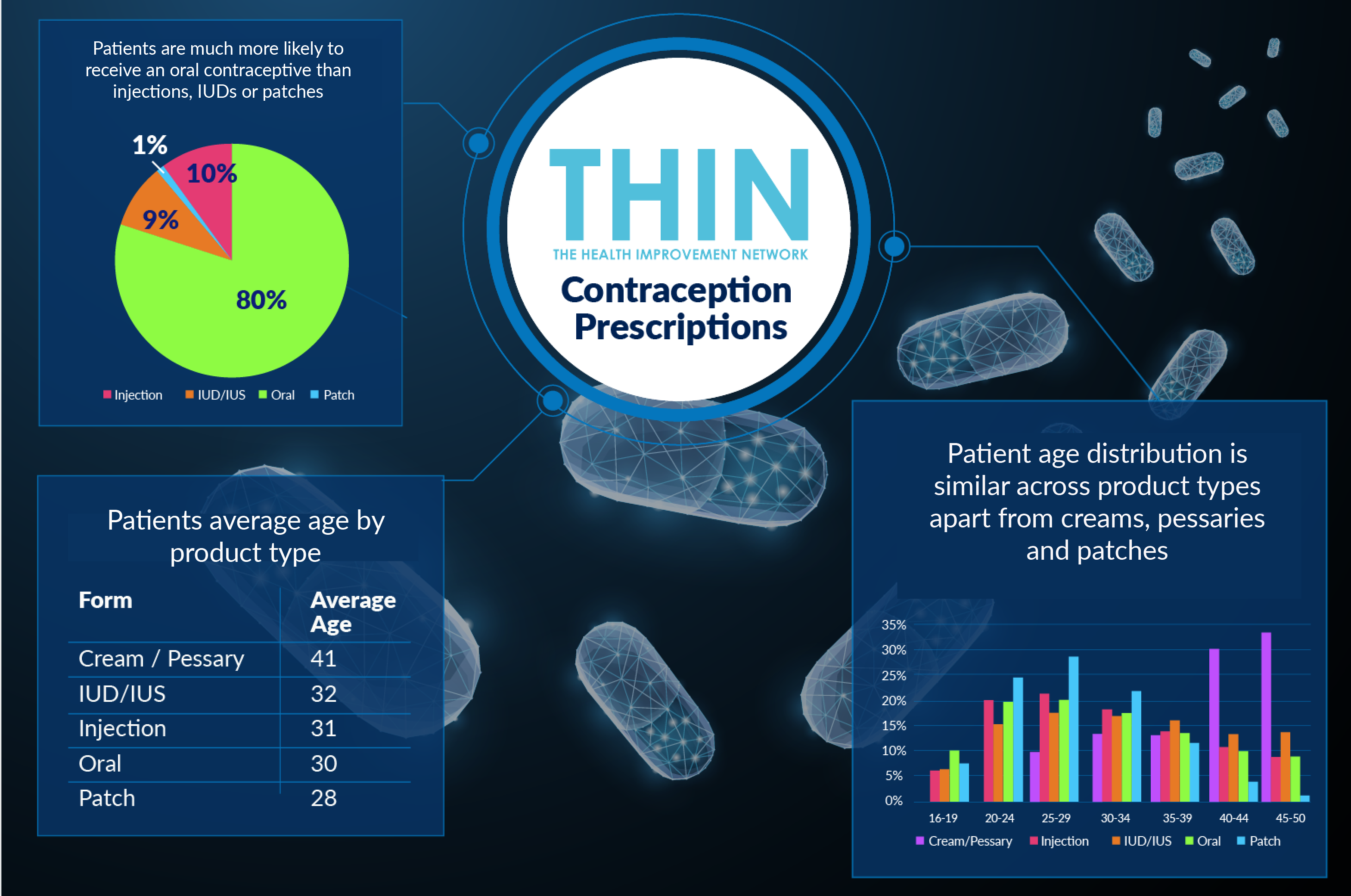
THIN’s anonymised, real-world population health data, shows that in the UK, 184,956 active patients have a prescription of a contraceptive. This equates to 22% of active patients, all of whom are female between the ages of 16 and 50.
Of these prescriptions, oral (a progestogen-containing product) contraceptives are prescribed significantly more than any other form of contraception, with 80% of active patients receiving this form of birth control. Although, patients’ average age changes by the type of product they receive, with patches being more favourable towards younger patients (with an average age of 28) and pessaries / creams more favourable amongst older patients (with an average age of 41). Contraceptive injections and intrauterine devices or systems account for approximately 19% of all contraceptive prescriptions.
Progestogen-only or Progestogen-combination?
There are 2 different types of progestogen-only pill:
- 3-hour progestogen-only pill (traditional progestogen-only pill) – must be taken within 3 hours of the same time each day
- 12-hour progestogen-only pill (desogestrel progestogen-only pill) – must be taken within 12 hours of the same time each day
Both types of pill are taken continuously, with no break between packs.
There are three different types of the combined pill:
- Monophasic 21-day pills - This is the most common type. Each pill has the same amount of hormone in it. One pill is taken each day for 21 days and then no pills are taken for the next 7 days.
- Phasic 21-day pills - Phasic pills contain 2 or 3 sections of different coloured pills in a pack. Each section contains a different amount of hormones. One pill is taken each day for 21 days and then no pills are taken for the next 7 days. Phasic pills need to be taken in the right order.
- Every day (ED) pills - There are 21 active pills and 7 inactive (dummy) pills in a pack. The two types of pill look different. One pill is taken each day for 28 days with no break between packets of pills. Every day pills need to be taken in the right order.

Of these two types of oral contraceptive, progestogen-only prescriptions are slightly more common than progestogen-combination pill – which also contains oestrogen, especially amongst older patients.
Comorbidities, Contraception & Pregnancy
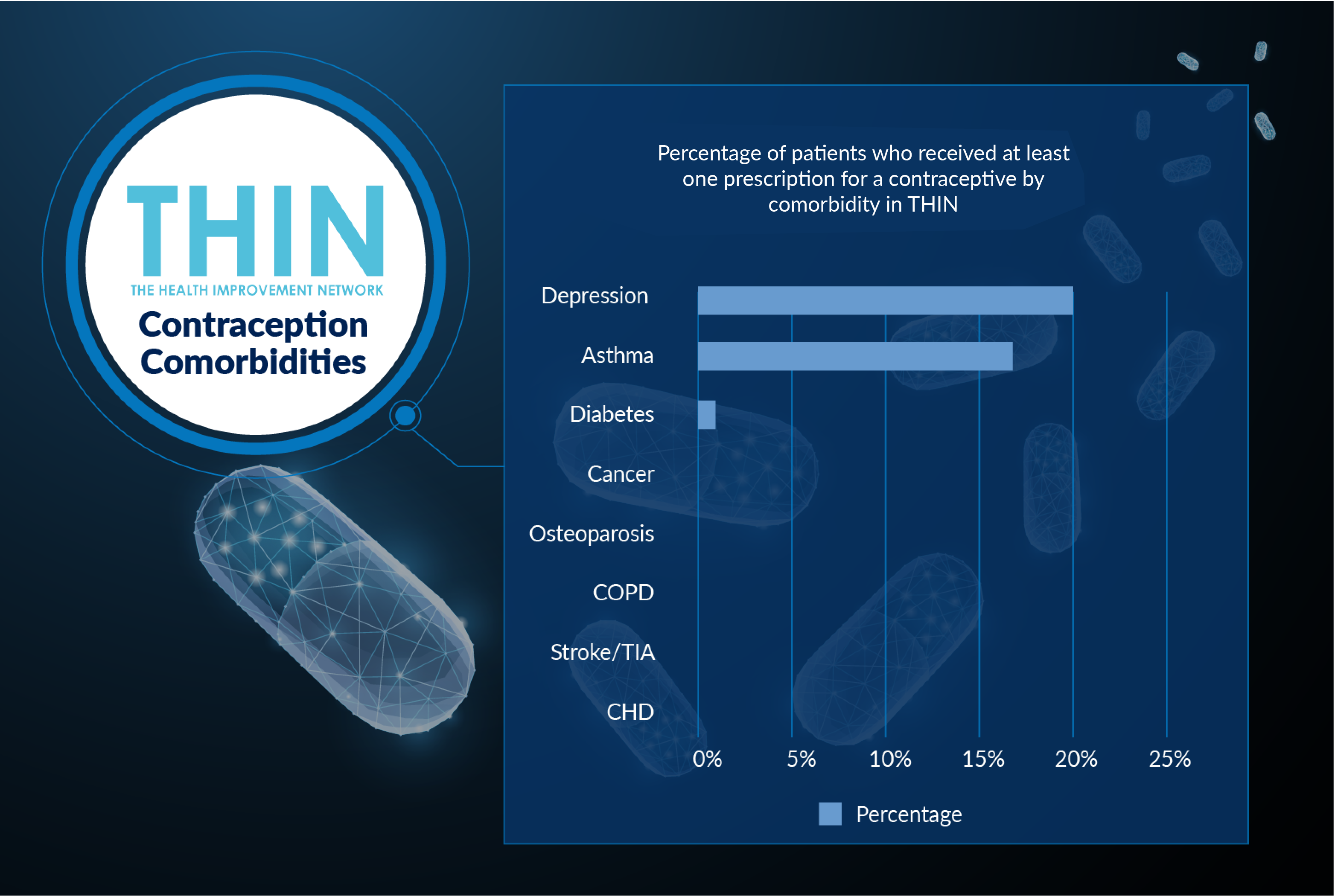
Although the number of comorbidities is relatively low, 20% of active patients are also diagnosed with depression, and 17% with asthma. These comorbidities may have a bearing on the type of contraceptive prescribed.
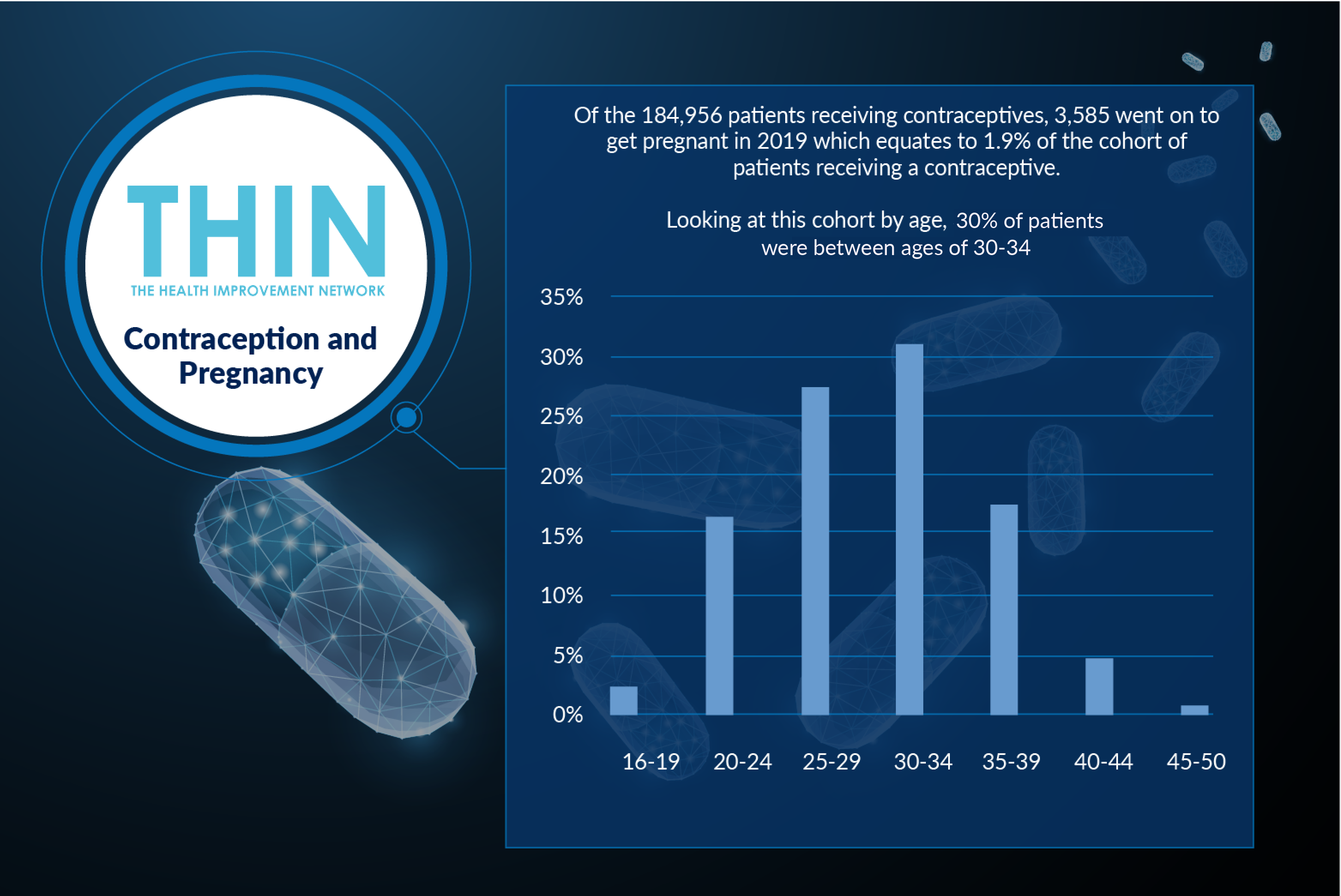
Of the 184,956 patients receiving contraceptives, 3,585 went on to get pregnant in 2019 which equates to 1.9% of the cohort of patients receiving a contraceptive. Looking at this cohort by age, 30%+ patients are aged between 30-34.
On World Contraception Day, it’s important to raise awareness around contraception and safe sex, and the choices available to patients so they can make informed decisions about their sexual and reproductive health.
The use of epidemiological health data such as THIN® will help provide deeper insight and help this informed decision-making, amongst both patients and clinicians.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.