Saving Lives with Better Targeted Research
Saving Lives with Better Detection/ Targeted Research
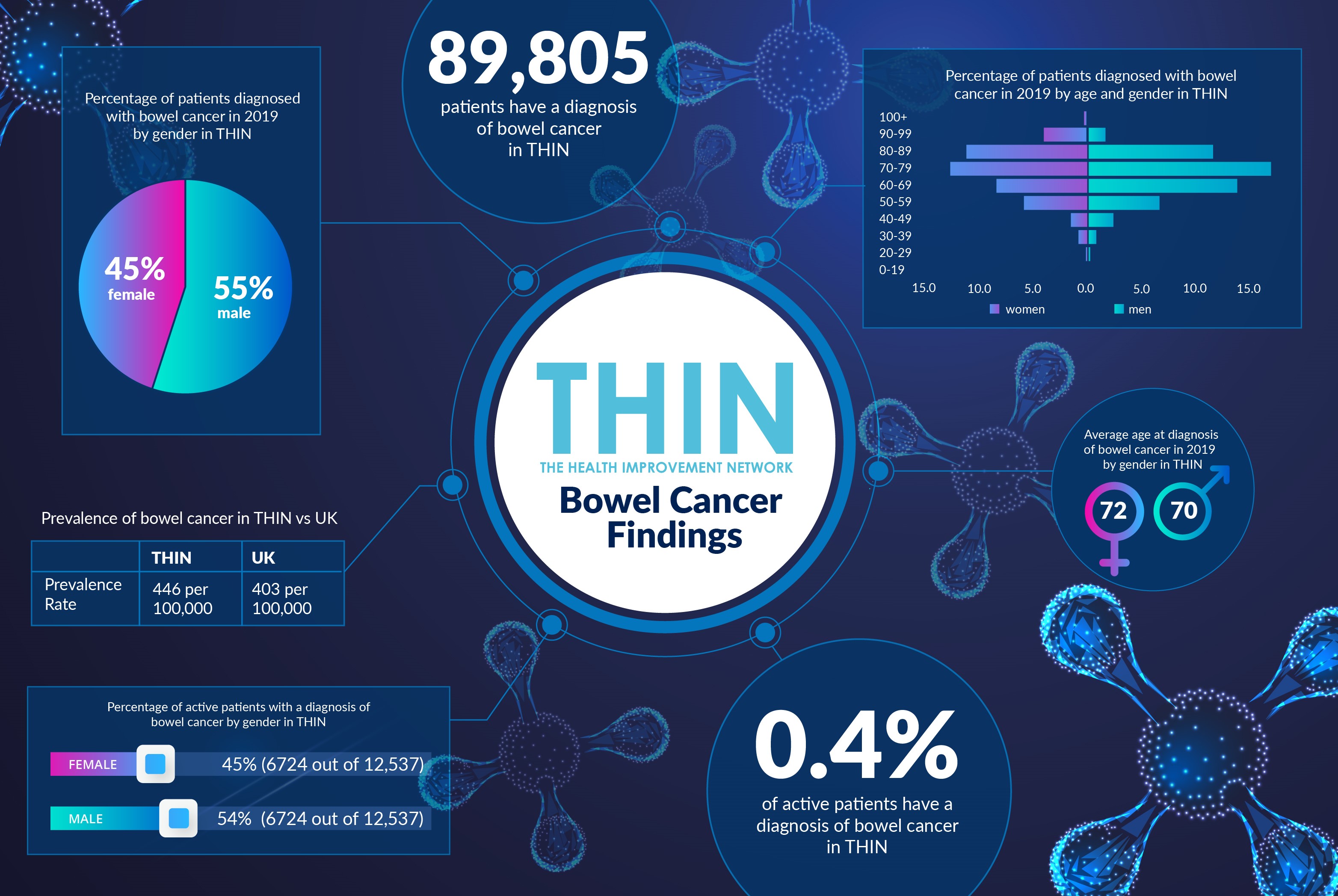
Bowel cancer is the UK’s second biggest cancer killer, with 16,000 people losing their lives to the disease every year in the UK, according to Bowel Cancer UK. While this is a cancer that responds well to treatment, the charity estimates that over the next 15 years around 332,000 more lives could be lost to the disease. The key to survival is early diagnosis; the challenge is that bowel cancer can be hard to detect.
During Bowel Cancer Awareness month, the goal is to both support the 268,000 people living in the UK today with bowel cancer and raise awareness of the importance of early diagnosis and screening.
Understanding Risks
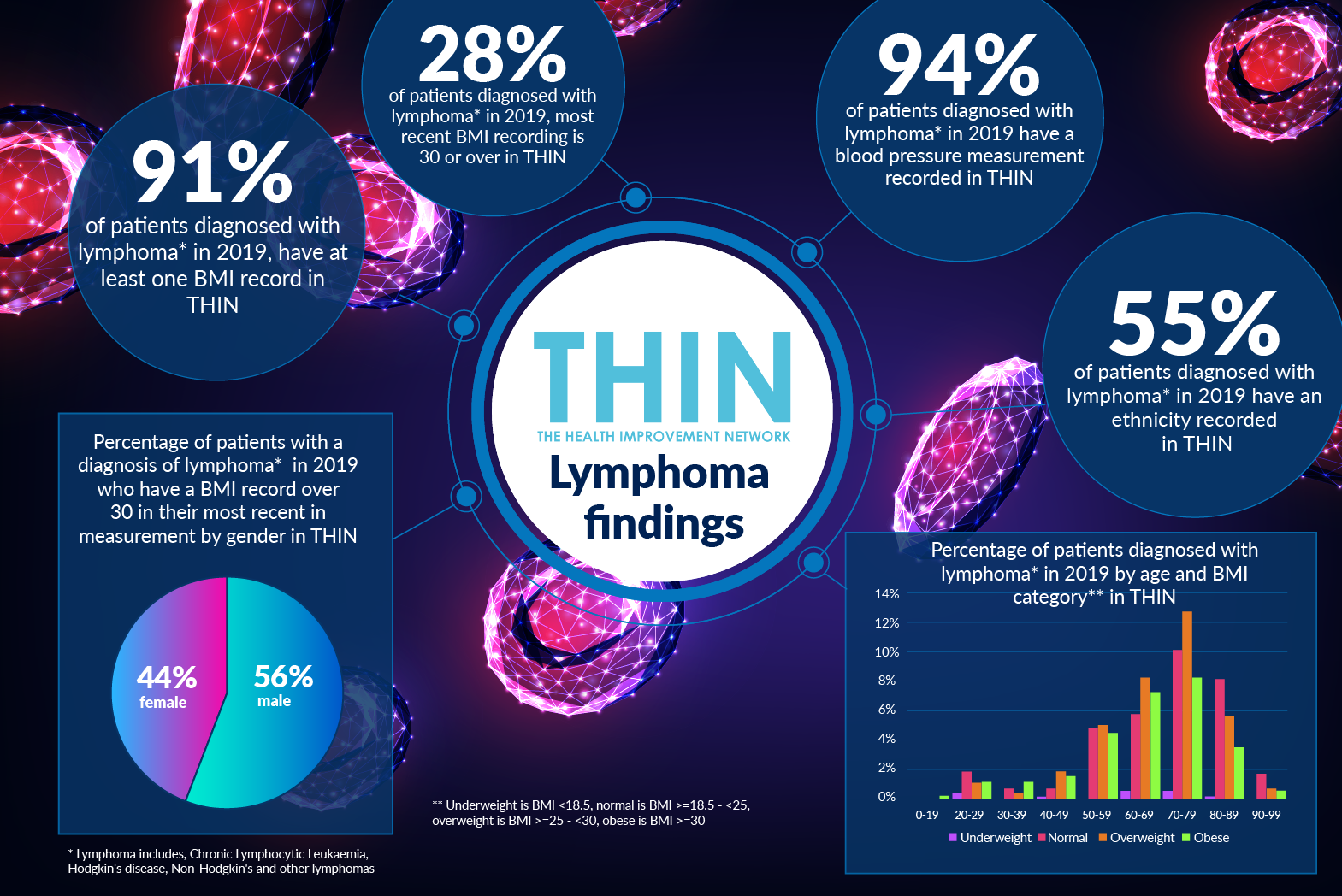
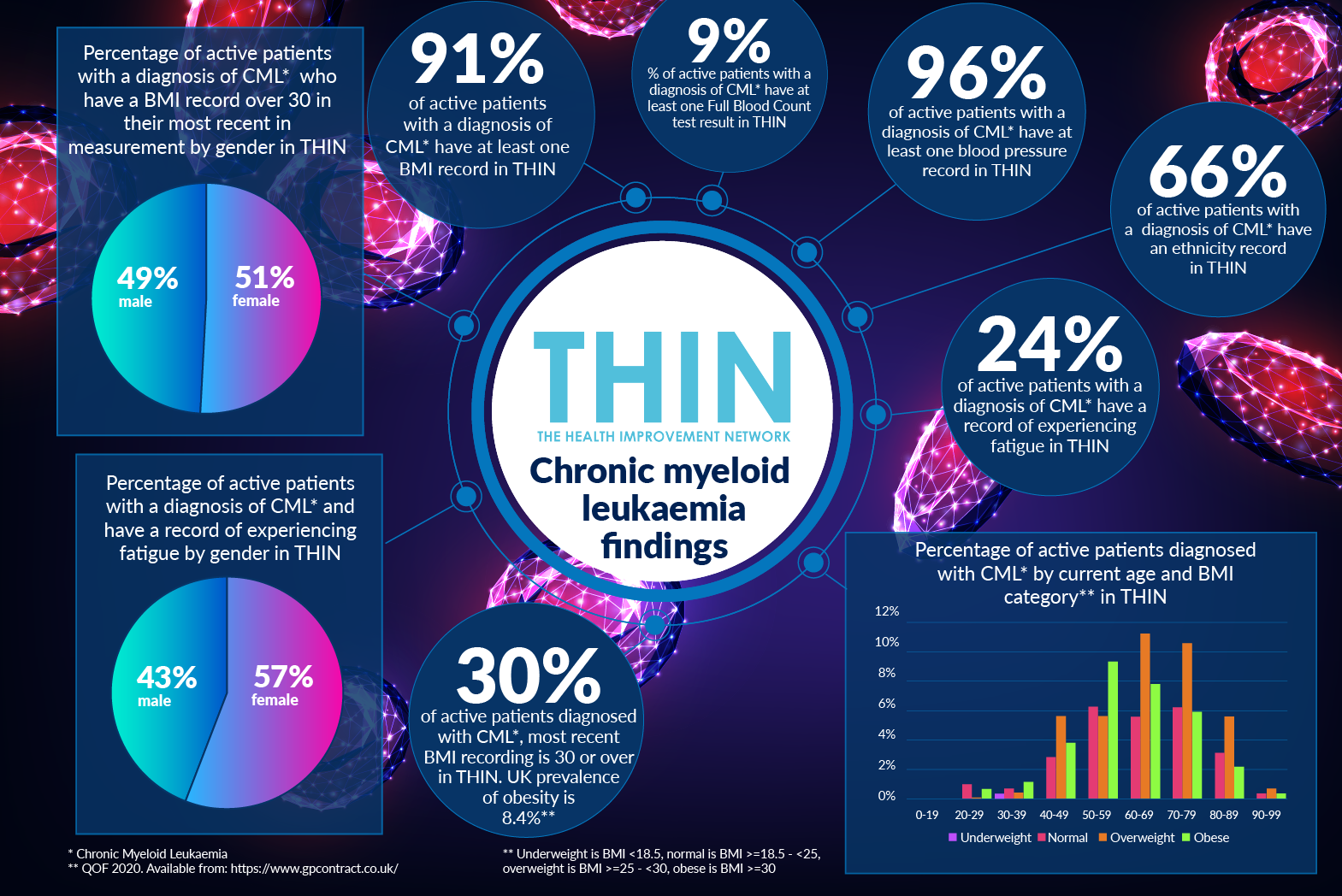
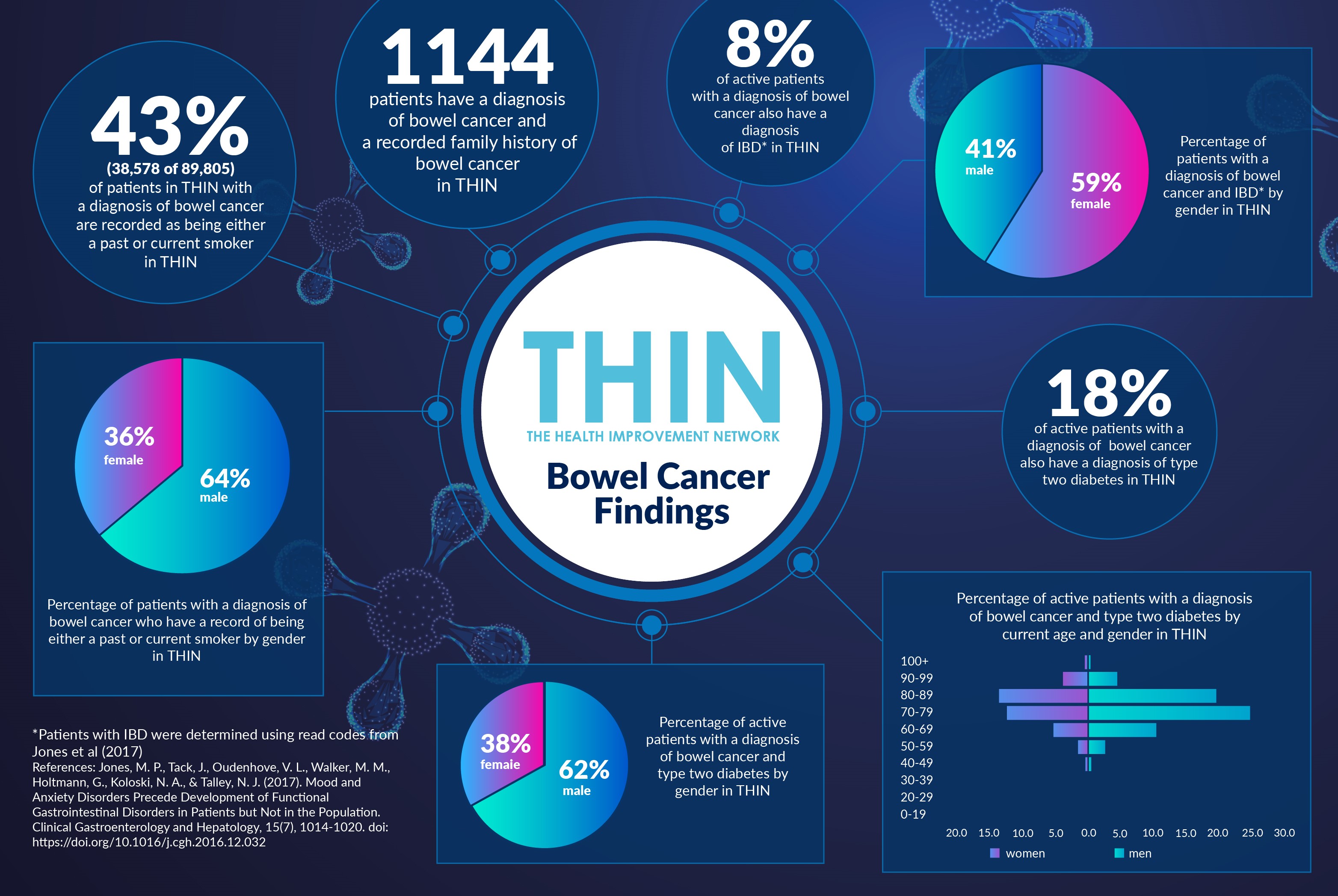
The risk factors associated with Bowel Cancer are well understood. The vast majority (94%) of new cases are diagnosed in people over the age of 50, and nearly six out of ten cases (59%) are diagnosed in people aged 70 or over. Additional factors include a strong family history of bowel cancer, a history of non-cancerous bowel polyps, or longstanding inflammatory bowel disease such as Crohn’s or ulcerative colitis. Lifestyle also has a quantifiable link to risk, with smoking, alcohol, poor diet, weight and Type 2 diabetes accepted factors.
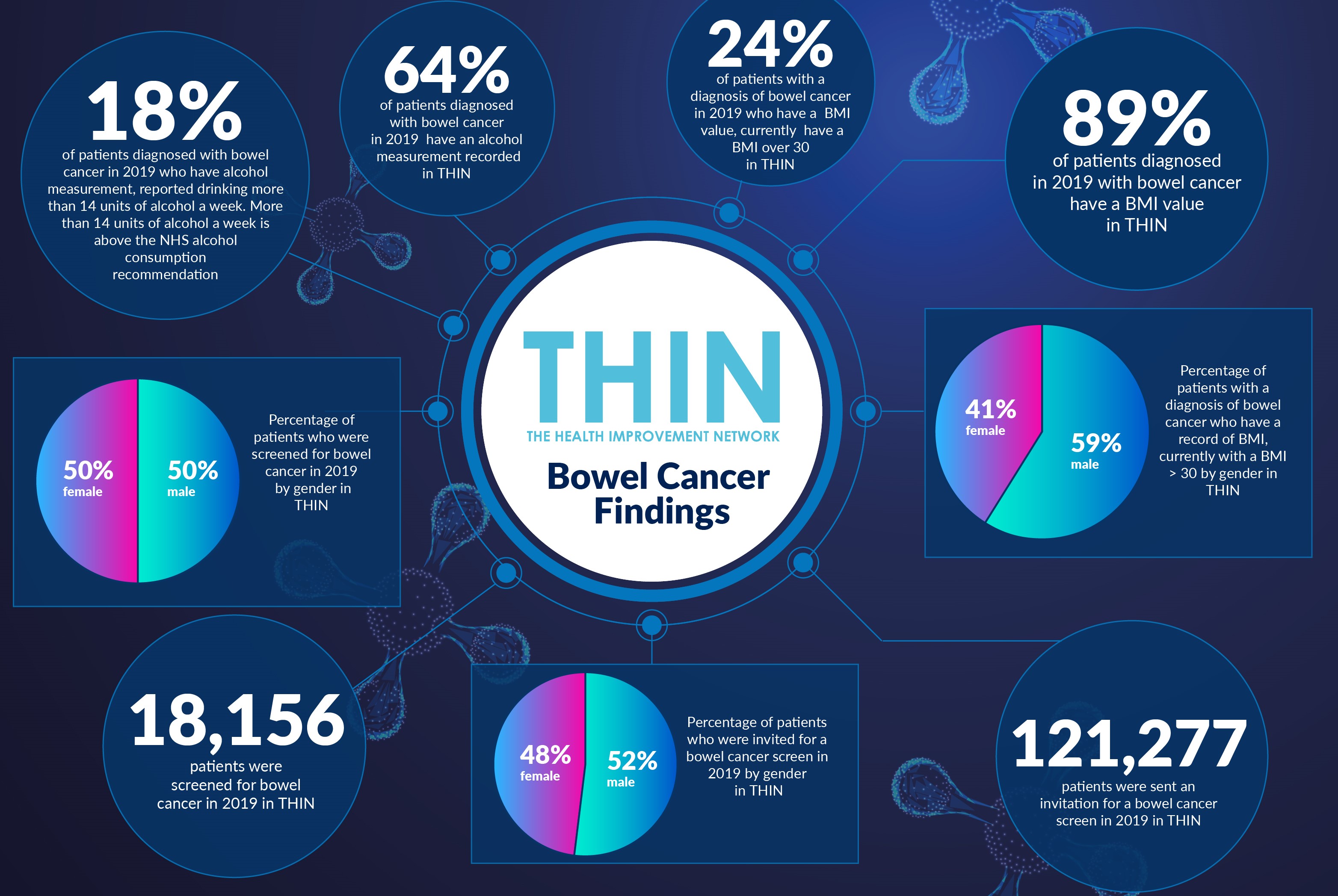
These comorbidities are confirmed in our analysis of The Health Improvement Network (THIN®), A Cegedim Database. Almost a fifth (18%) of active patients with a diagnosis of bowel cancer also have a diagnosis of Type 2 diabetes in THIN®; 43% are recorded as being either a past or current smoker and 24% of patients with a diagnosis of bowel cancer in 2019 who have a BMI value in THIN®, currently have a BMI over 30. In addition, 18% of patients diagnosed with bowel cancer in 2019 who have alcohol measurement, reported drinking more than 14 units of alcohol a week - above the NHS alcohol consumption recommendation.
As Bowel Cancer UK stated in its ‘Finding the Key to the Cures’ report, “To spot cancers early, we need a better understanding of who may be at particular risk of developing the disease and to monitor them regularly and effectively. We need to understand all the individual components that work together to increase a person’s risk of bowel cancer.”
Screening Programmes
Bowel Cancer UK estimates that nearly half of all bowel cancers are due to lifestyle factors. Adopting a healthier lifestyle, including more fibre in the diet, reducing red meat consumption, changing the gut microbiome and calorie restriction are all believe to help prevent the disease.
Despite the influence of diet, exercise and alcohol consumption, the established screening processes across the UK are age related. In England, Wales and Northern Ireland people over the age of 60 are invited to take part in bowel cancer screening; in Scotland, screening starts from age 50. But bowel cancer can affect anyone of any age: more than 2,500 new cases are diagnosed each year in people under the age of 50.
Furthermore, take up of the screening could be higher – as our THIN® analysis reveals. In 2019, 18,000 people have a record of being screened; while 116,000 are recorded as not responding to their screening invitation in 2019.
A number of these patients will have been referred for screening by a GP due to possible symptoms, such as blood in faeces or unexplained weight loss, rather than simply taking the recommended biannual test.
GPs are being urged during Bowel Cancer Awareness Month to raise awareness of the symptoms and to reinforce the value of prevention – such as lifestyle changes – as well as encouraging the uptake of bowel cancer screening.
Genetic and Lifestyle Influence
There is growing research to discover the genes that drive bowel cancer in a diverse cross-section of society. While this is incredibly exciting, Bowel Cancer UK is also calling for more insight into the precise relationship between genetic, environmental and lifestyle factors linked with bowel cancer risk across the population as a whole. A recent study even suggests the Bowel Cancer Screening Programme should consider including lifestyle and genetic information so that invitations to join the screening programme are tailored based on a person’s risk.
This is where THIN® can be so powerful in joining up the dots. Our data provides a clear representation of community and population health which, when combined with proactive strategies for improving population health, including prevention strategies, can deliver more effective models of care for patients.
Improving awareness of the importance of bowel cancer screening is invaluable; but better understanding of the influence of lifestyle and environmental issues that influence bowel cancer risk are essential in both reducing risk and enabling early diagnosis.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.