World Diabetes Day 2020
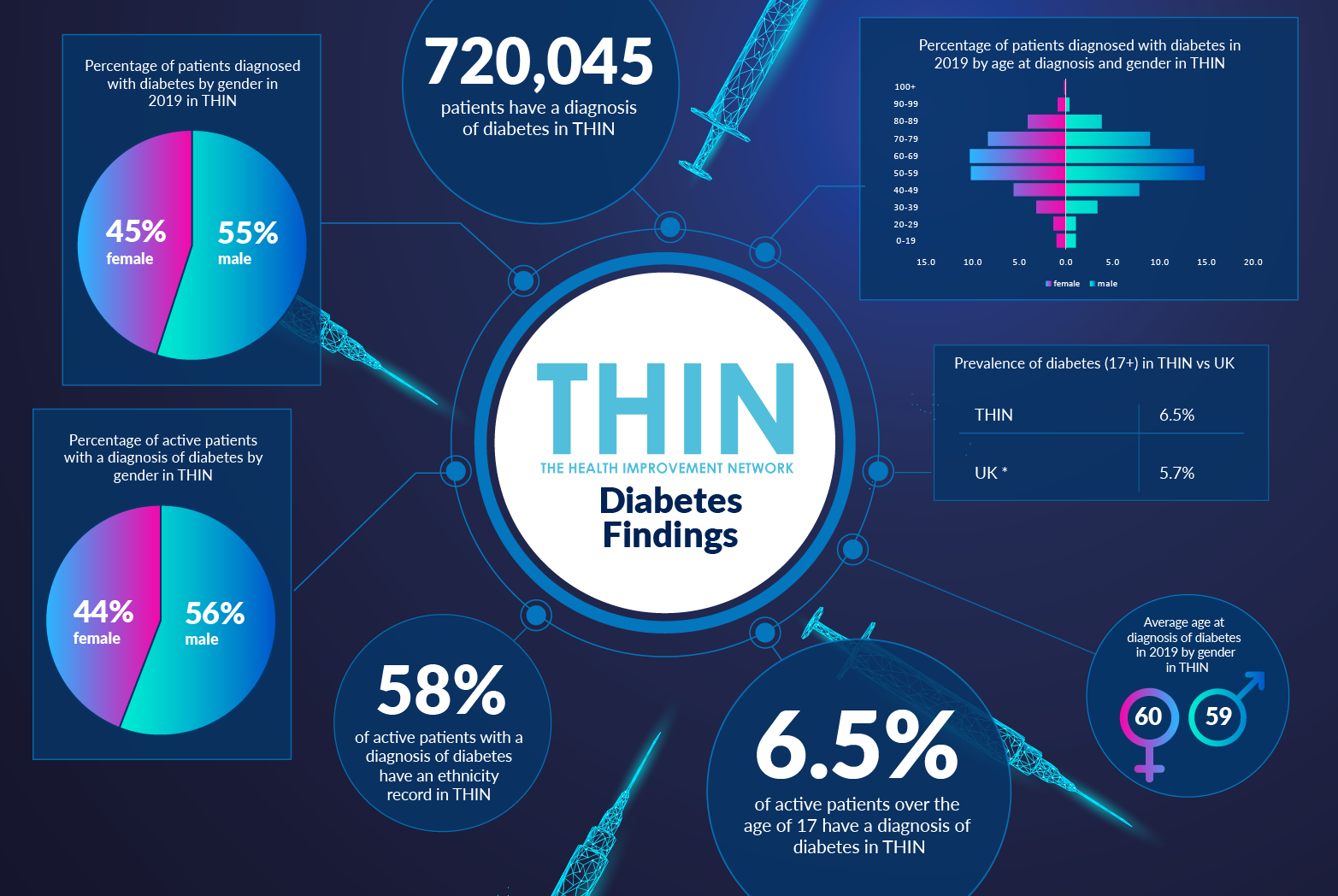
One in ten people are living with diabetes, a fact that has been highlighted this year by the COVID-19 pandemic. While age is by far the biggest baseline risk for COVID-19, people with diabetes have been found to be more at risk of dying that others: individuals with Type 1 diabetes have three and a half times the risk, and those with Type 2, twice the risk.
Body weight is also a COVID-19 risk factor, reinforcing the fact that it has never been more important for individuals to maintain a healthy lifestyle. Given the spotlight on the need for a balanced diet, more exercise and better sleep, this year’s World Diabetes Day campaign on 14th November is highlighting the role of nurses in the prevention and management of diabetes.
Living with Diabetes
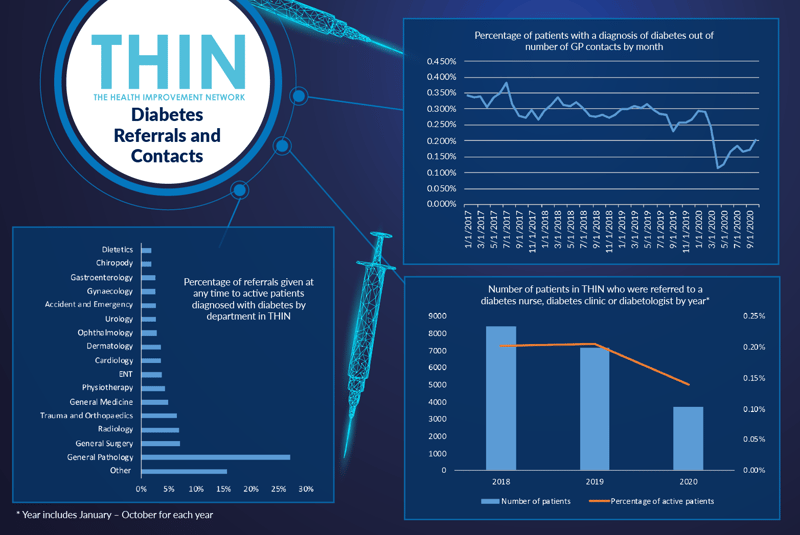
There is no question that diabetes care has been very different this year – and researchers have been keen to understand the implications for people living with diabetes. In a global survey of more than 7,000 people with type 1 diabetes, 30% reported that the pandemic had affected their healthcare access due to cancelled physical appointments – and 9% said that they hadn’t had any contact from their doctors over the duration of the study. Many, however, have adapted to telemedicine and would be happy to conduct some elements of diabetes care remotely in the future.
This global research is backed up by findings from The Health Improvement Network (THIN®), a Cegedim database, which revealed a dramatic drop in GP contacts for diabetes patients in the UK this year. GP contacts fell from 0.3% in January 2020 to just 0.1% in March 2020. Numbers have begun to climb back slowly, but even by October the figure had only just got back to 0.2% - and that was before the second lock down.
Furthermore, the number of patients in THIN® referred to a diabetes nurse, diabetes clinic or diabetologist by year* also dropped from 0.20% in 2018 and 2019, down to 0.14% in 2020. This reflects concerns raised as a result of the UK National Diabetes Audit which revealed that less than 10% of people newly diagnosed with type 2 diabetes attend a diabetes structured education (DSE) course.
Diabetes Support
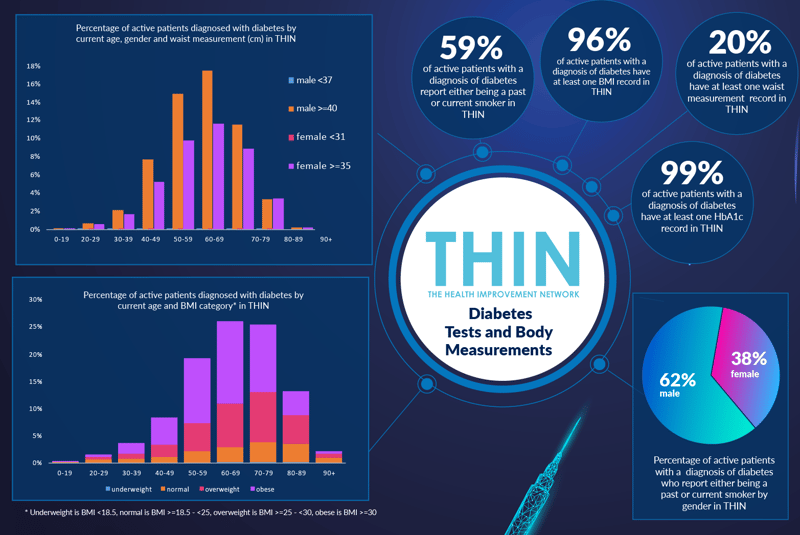
When improving lifestyle can play such a vital role in managing diabetes this lack of clinical interaction is a concern. Well over half (59%) of active patients with a diagnosis of diabetes report either being a past or current smoker in THIN®. The link between weight and diabetes is also clear: 96% of active patients with a diagnosis of diabetes have at least one BMI record in THIN® and while 15% of individuals with a BMI in the normal range are diabetic, the vast majority of patients are overweight or obese.
Waist measurement is increasingly preferred as an indicator of weight – and 20% of active patients with a diagnosis of diabetes have at least one waist measurement record in THIN®. Again the figures underline the link with weight and a diagnosis of diabetes: men with a waist measurement of over 40 inches and women with a waist measurement of over 35 inches dominate in every age group.
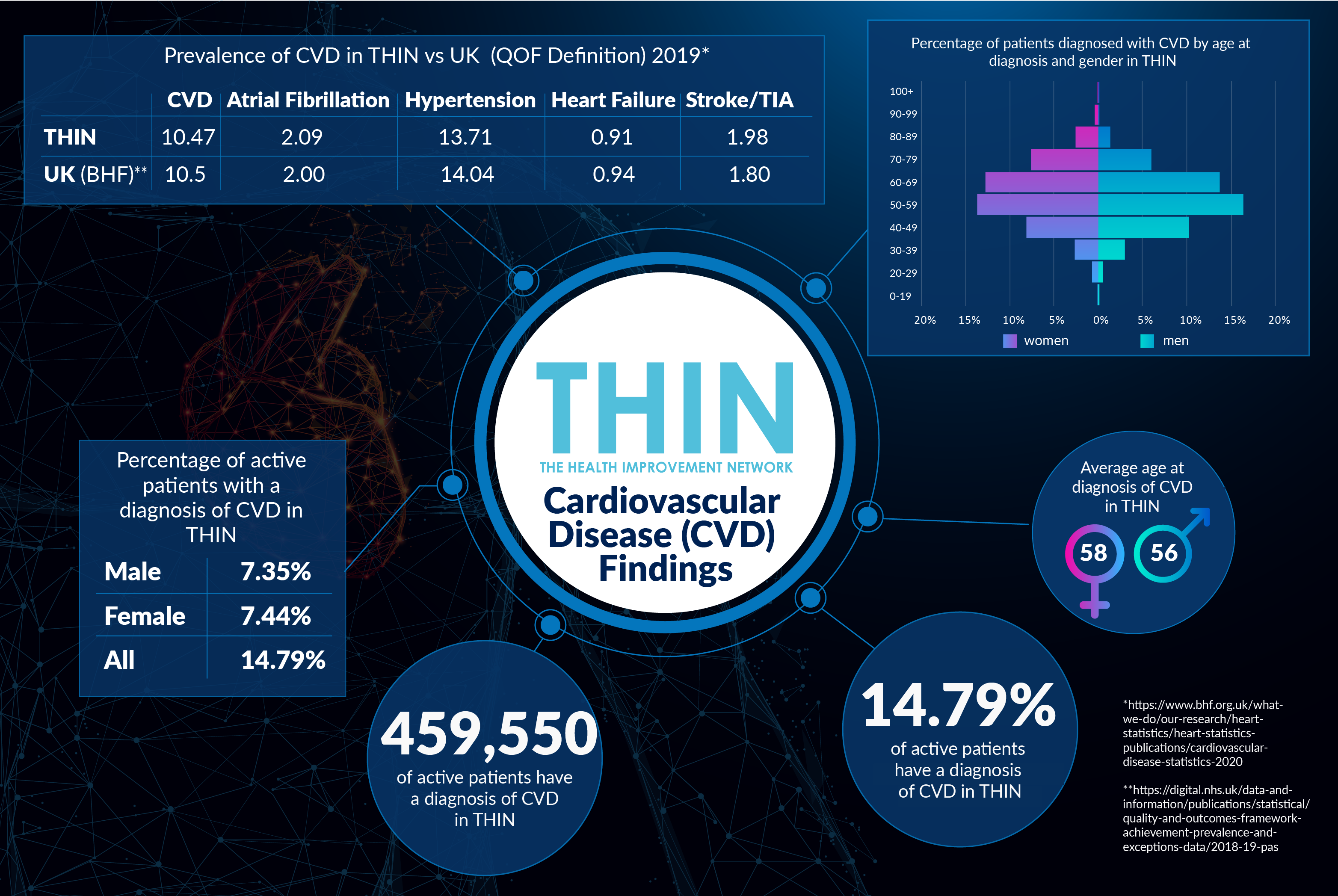
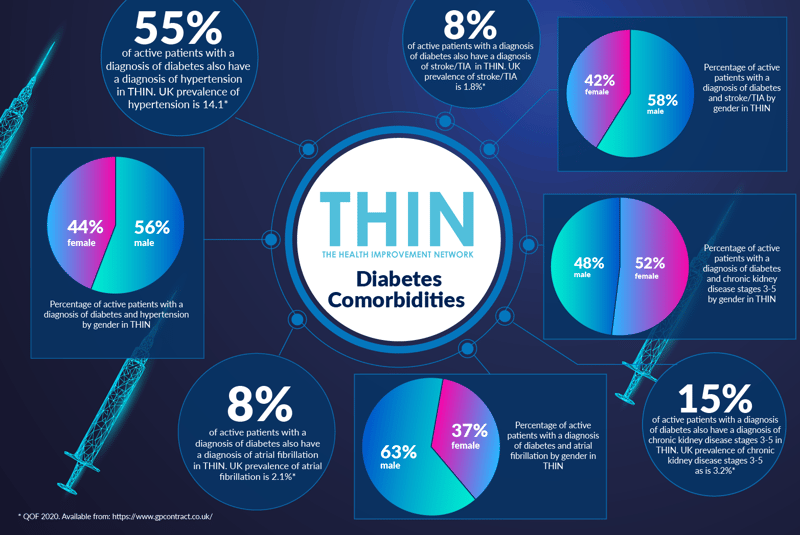
COVID-19 is far from the only additional health concern affecting those living with diabetes. Analysis of THIN® data confirms a number of comorbidities, including hypertension, atrial fibrillation, stroke/TIA and chronic kidney disease (CKD). While the prevalence of hypertension in the overall THIN® patient population is 14.1%, the majority (55%) of active patients with a diagnosis of diabetes also have a diagnosis of hypertension.
These comorbidities affect diabetes treatment – while THIN® data confirms that 51% of active patients with a diagnosis of diabetes have received at least one prescription for metformin in 2019, this drug is not suitable for those with liver or kidney problems or those being treated for heart failure or recent heart attack.
A recent study suggests the use of SGLT2 inhibitor empagliflozin can reduce risk of hospitalisation from heart failure by 28%, both in people with and without type 2 diabetes. THIN data confirms that 11 % of active patients with a diagnosis of diabetes have received at least one prescription for a SGLT-2 inhibitor in 2019 in THIN®.
Prioritising Access to Diabetes Nurses
Improving diet and increasing exercise is recognised as having a very significant impact for those with type 2 diabetes and the Diabetes Specialist Nurses (DSNs) are crucial in providing good patient care and promoting self-care management. This is where THIN® data is so valuable – supporting proactive referral of individuals with diabetes to the correct community support services while also contributing to the improved population health strategy and planning that is required to address the continual rise in diabetes, with the associated implications for day to day living.
* Year includes January – October for each year
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.