Understanding Heart Disease to Power Better Pathways and Safer Models of Care
Cardiovascular disease (CVD) is the number one cause of death on the planet. An umbrella term for conditions that affect a person’s heart or circulation, it has many causes: from obesity, diabetes, high blood pressure and cholesterol, to stress, smoking, air pollution, and rare and neglected conditions such as Chagas Disease and cardiac amyloidosis.
In the time of COVID-19, CVD patients are faced with a double-edged threat. Not only are they more at risk of developing severe forms of the virus, but they may also be afraid to seek ongoing care for their hearts.
On World Heart Day, 29th September, it’s all about enabling discoveries that improve the lives of those people living with heart disease and powering more effective models of care for those at risk.
COVID-19 and Cardiovascular Disease
CVD patients are more susceptible to severe COVID-19. However, with research indicating that the number of heart attacks detected and treated during the early part of the pandemic fell by 40% - and that the number of deaths from the most common type of heart attack rose by 40% during lockdown – advice from the World Heart Federation rings true: “For people who have underlying health conditions such as heart disease, the message has to be that your hospital, emergency room, or doctor’s surgery is safe, and if you need to go, you should. The risks of heart attacks and stroke far outweigh the risks of contracting COVID-19 and time is truly of the essence when heart troubles hit.”
Symptoms & Risk Factors
Symptoms of CVD can vary based upon a patient’s condition and can include chest pain; pain, weakness or numb legs and/or arms; breathlessness; very fast or slow heartbeat, or palpitations; feeling dizzy, lightheaded or faint; fatigue; and swollen limbs.
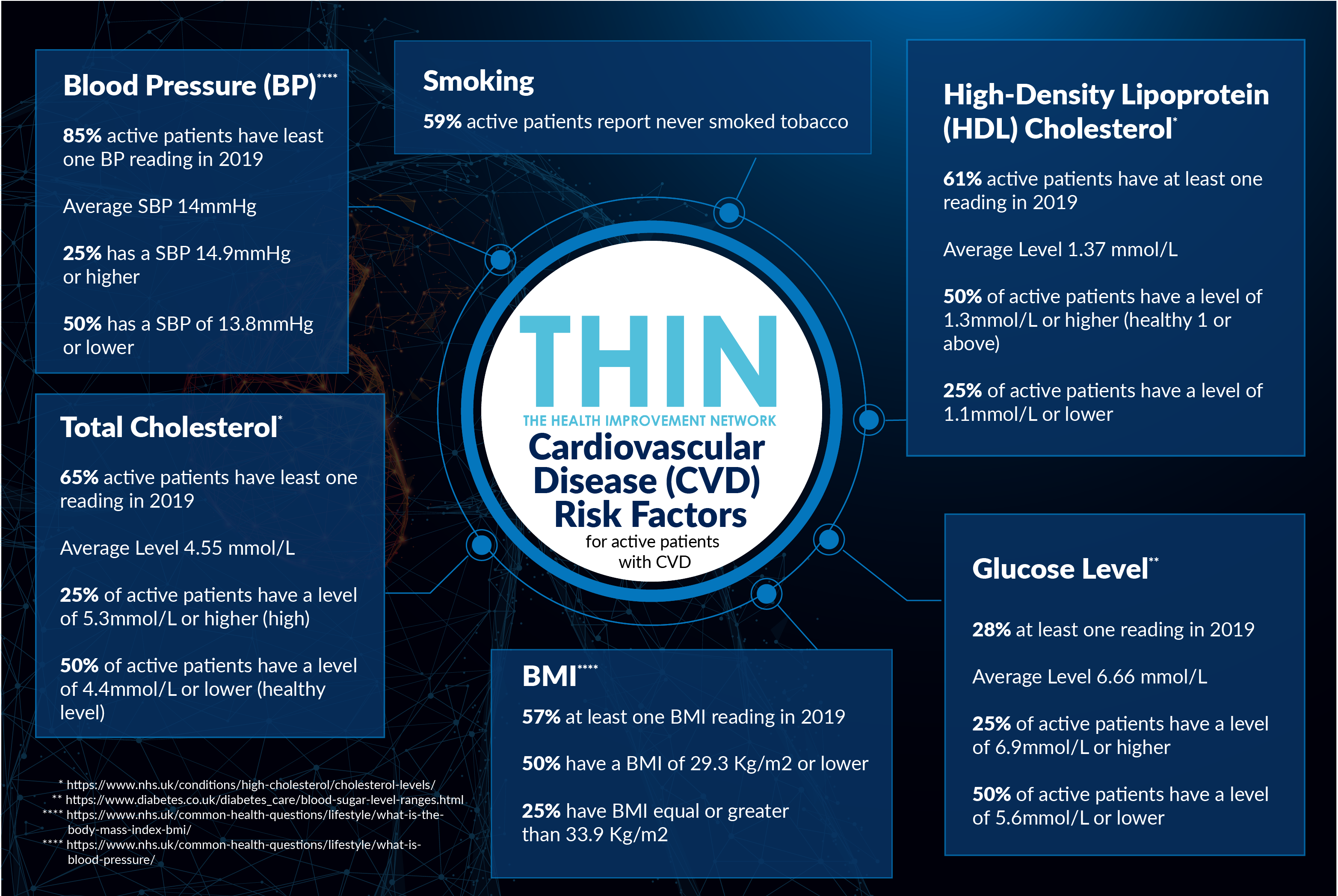
The exact causes and risk factors of CVD are both unclear, as well as many and varied. Certain risk factors cannot be controlled, such as age (risk generally increases with age), gender (men are likely to develop CVD at a younger age, though women are rapidly catching up) and family history. However, other risk factors that can be controlled through medication and / or changes in lifestyle include: cholesterol; activity level/exercise; smoking; weight/BMI; blood pressure; and glucose level. Increasing understanding of how better management of these controllable risk factors can improve a patient’s condition, is key to powering better pathways and improved outcomes.
Understanding Comorbidities
Comorbid conditions are very common in patients with CVD, even in younger age groups. Comorbidities typically include hypertension; coronary heart disease (CHD); diabetes; and Atrial Fibrillation (AF), amongst others. Indeed, today comorbidity tends to be considered the rule rather than the exception, so increasing awareness and improving guidance for patients with comorbid conditions is crucial in order to prevent adverse health outcomes, improve quality of life, increase efficiency, and reduce costs.
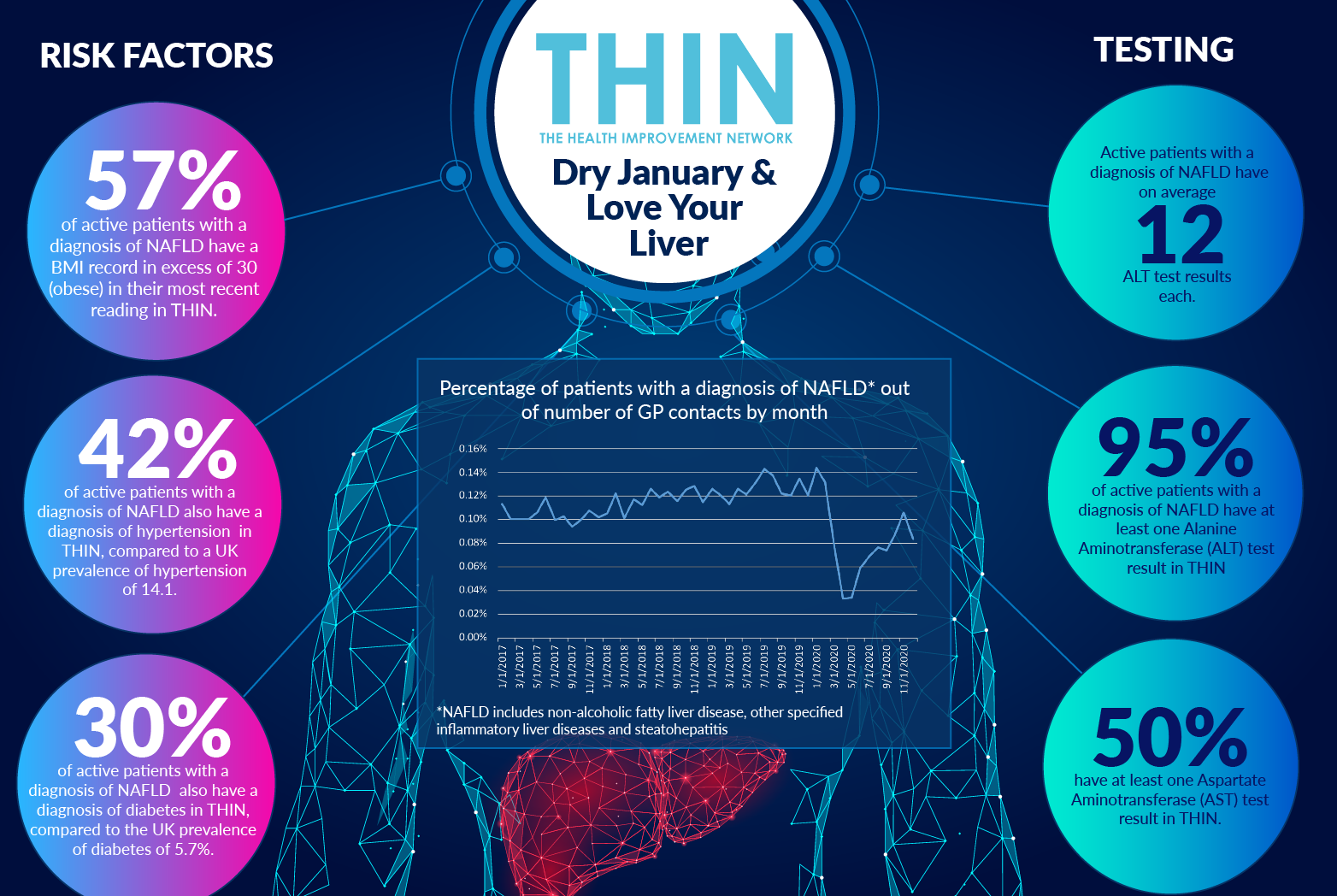
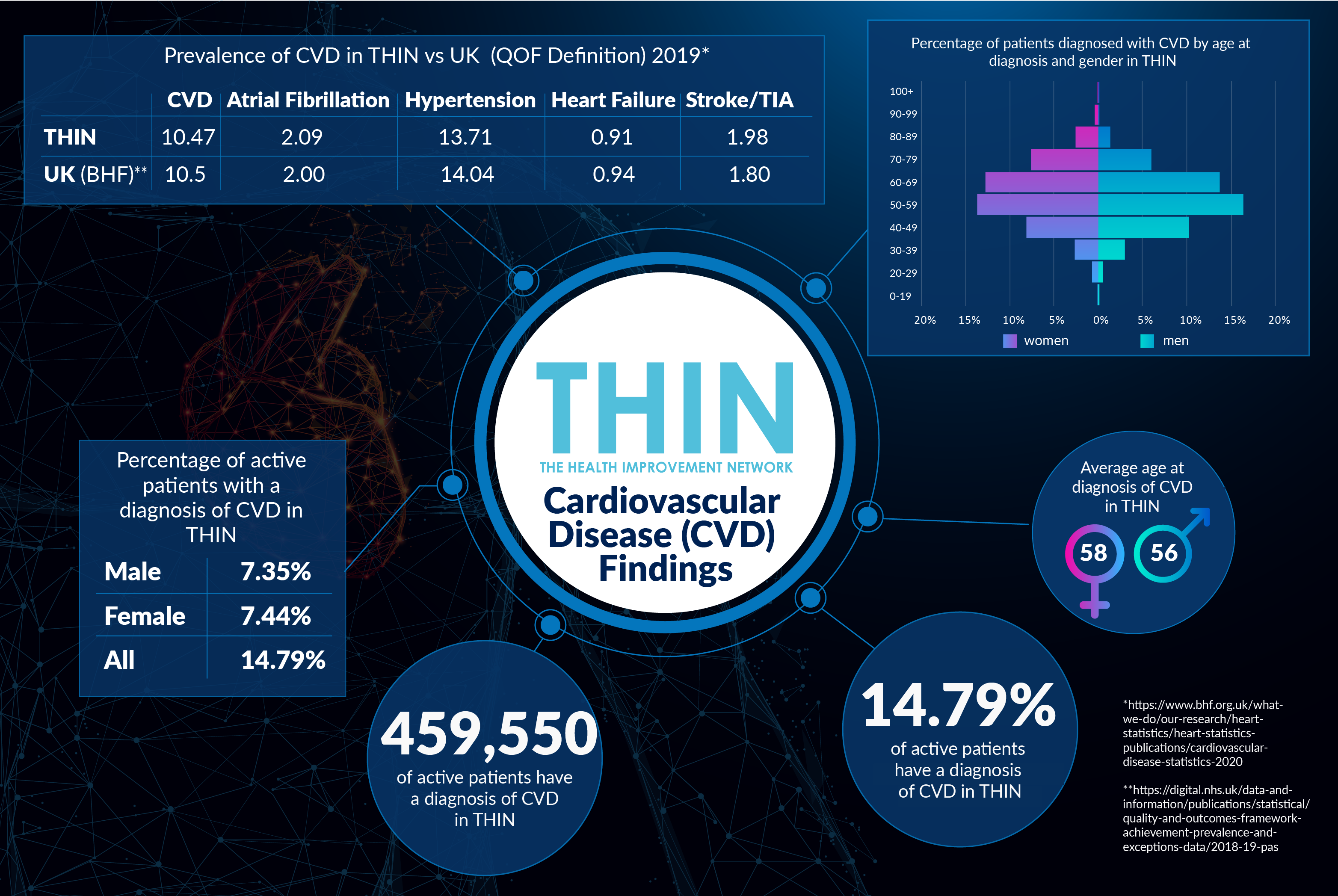
Research continues globally, which is why population health data, as provided by THIN®, is vital. With 459,550 active diagnoses of CVD – representing nearly 15% of UK patients – analysis confirms the prevalence of comorbidities and the slight male bias.
Within THIN®, men are more likely to be diagnosed at a younger age (58) than women (56), though the number of women diagnosed over the age of 70 is noticeably higher than the number of men, making the total number of women diagnosed slightly higher (7.44% of cases versus 7.35%). Moreover, of the active patients diagnosed with CVD, nearly 86% have hypertension as a comorbidity, with men again typically diagnosed at a younger age than women.
THIN® data also confirms that other common comorbidities include CHD (21.69%); diabetes (21.55%); and AF (9.67%).
Understanding Risk Factors
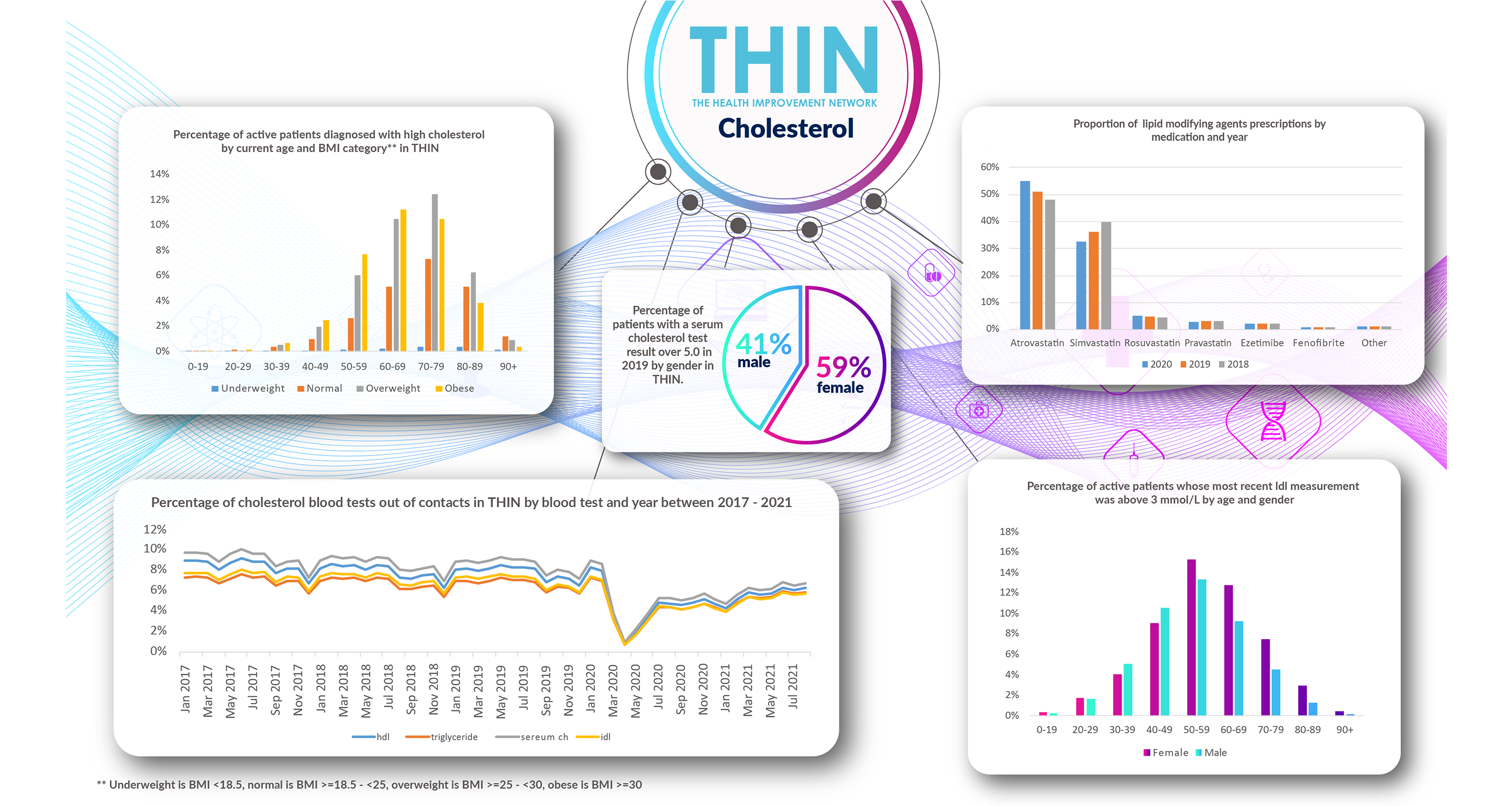
Of the risk factors recorded in THIN® during 2019, all have a part to play. Unsurprisingly, given the high percentage of comorbid hypertension, active patients’ average systolic blood pressure was 140mm/Hg, considered high according to NHS guidance. 25% of active patients also recorded a total cholesterol level of 5.3mmol/L (compared to a recommended healthy level of 5mmol/L or lower) and an HDL cholesterol level of 1.1mmol/L or lower (against a recommended healthy level of 1mmol/L or above).
Similarly, BMI or weight is a factor, with 50% of active patients who had their BMI read during 2019 recording a BMI of 29.3 or lower, and 25% recording a BMI of 33.9 or above. With NHS guidance classifying that a BMI of 25 and above in the ‘overweight’ category, and 30 or above as ‘obese’, clearly more could be done to help these patients understand the impact of weight on their condition and ways in which they can address it.
Powering Better Pathways
Although we cannot cure heart disease, we can make it better. Most forms of CVD are very treatable today, be that through recommended lifestyle changes and medication to reduce risk.
However, given the number of risk factors and comorbiditites, the patient pathway for CVD is not straightforward. Moreover, with the statistics around decreased GP and hospital attendance for potential heart attacks well-publicised, the number of at risk patients is likely to see a rapid increase over coming months – with the potential of a second wave of COVID-19 further impacting diagnoses and treatment further down the line.
The use of epidemiological health data such as THIN® will help connect the dots. Better insight into comorbidities and risk factors will help not only with earlier identification and awareness but also enable discoveries that can powering safer, more effective models of care that improve people’s lives.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.