Addressing Mental Health Stigma on World Bipolar Day
Awareness of mental health has never been higher. But for those with disorders such as bipolar -estimated to be more than one million people in the UK – the escalated stress levels during the current pandemic crisis is likely to have serious implications.
While bipolar disorder can affect anyone, regardless of age or background, rates may be higher among particular groups such as young adults, those who are unemployed or in receipt of benefits, and those who live alone. These relationships may be bi-directional, which means that stressful circumstances may be a risk factor for developing bipolar disorder. With so many people fearing for their jobs and forced to self-isolate, difficulties in managing bipolar symptoms cannot be ignored.
Understanding Bipolar
Bipolar has a huge impact on families and friends and many people with bipolar continue to lack the basic support and treatment needed to live well with the condition. Which is why World Bipolar Day on 30th March 2020 is focused on raising awareness, improving sensitivity and eliminating social stigma.
Bipolar disorder is characterised by recurring episodes of extreme or overwhelming mood. Symptoms will depend on which type of extreme mood (referred to as depression and mania) is experienced and may not be the same for everyone, or for every episode. It is, however, a growing issue. Young people are more likely to screen positive than older people – and estimates of the global prevalence of bipolar disorder is between 1 and 2%, even as high as 5%.
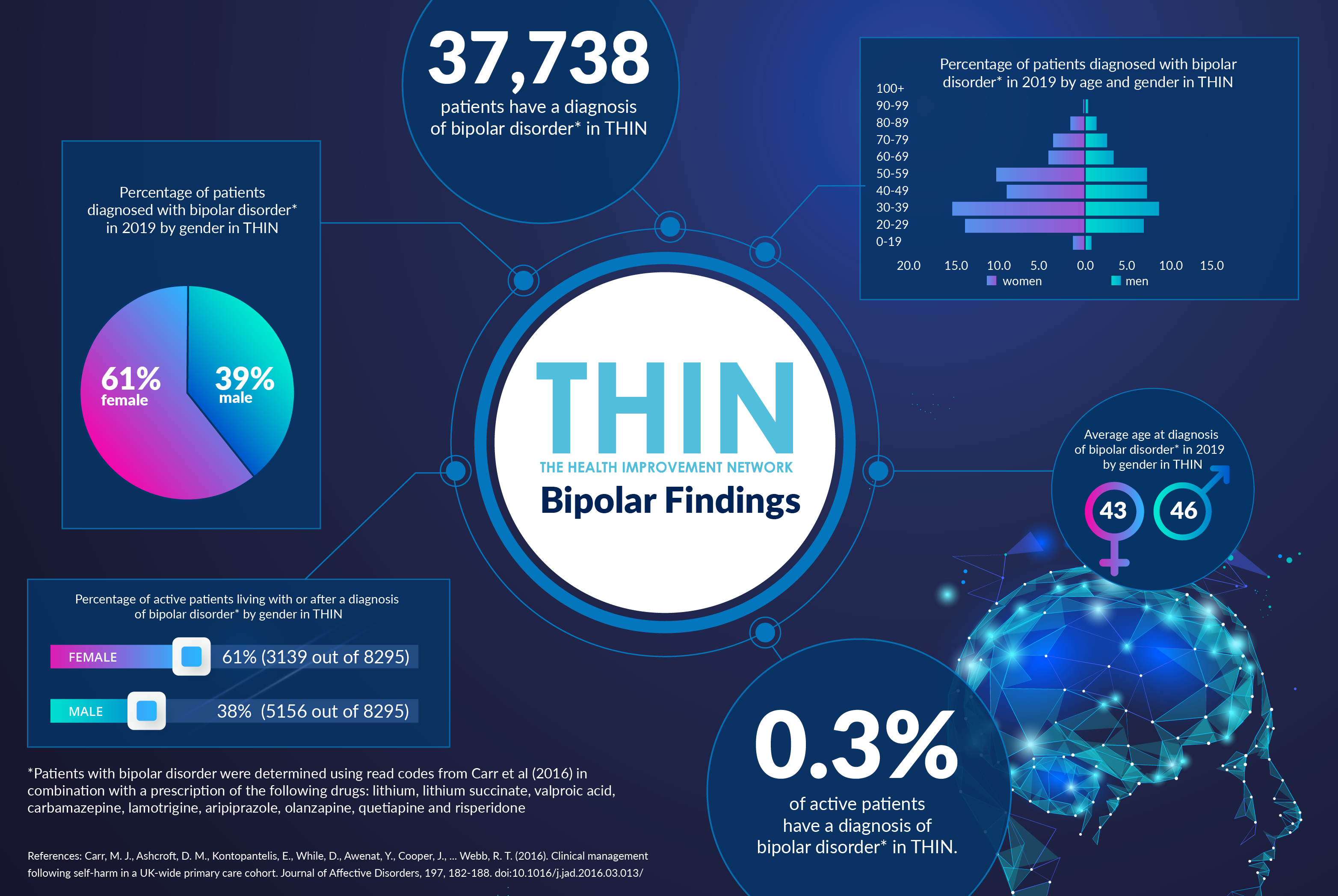
Gender Differences
While bipolar disorder affects men and women in roughly equal numbers, there are gender differences in the ways the illness manifests. Women with the disorder tend to have more depressive and fewer manic episodes and are more likely to have bipolar II. A man's first experience with bipolar disorder may be in a manic state; women tend to first experience a depressive state and appear to be more prone than men to rapid-cycling.
However, our analysis of The Health Improvement Network (THIN®), A Cegedim Database, has confirmed a difference in diagnosis by gender: with 61% of patients diagnosed with bipolar disorder* in 2019 by gender in THIN are female. These figures could reflect the gender bias that occurs in the treatment of psychological disorders, with doctors more likely to diagnose depression, one of the features of bipolar, in women compared with men, even when they have similar scores on standardized measures of depression or present with identical symptoms.
Gender differences also exist in the way individuals seek help for psychological disorder: women are more likely to seek help from and disclose mental health problems to their primary health care physician while men are more likely to seek specialist mental health care and are the principal users of inpatient care. Men are also more likely than women to disclose problems with alcohol use to their health care provider.
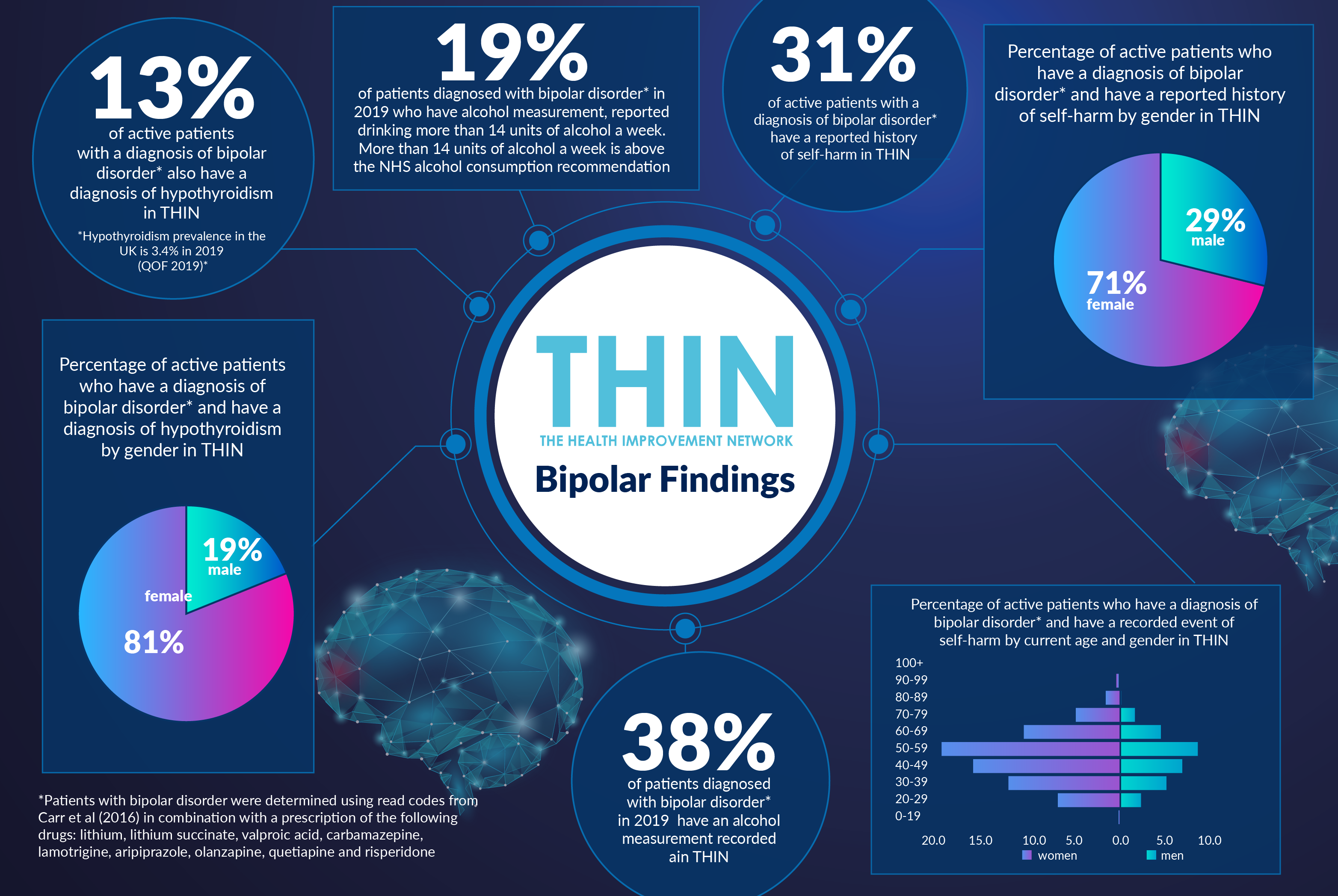
Research also suggests that abnormal thyroid levels as such imbalances are more common in women than men, with a link between rapid cycling bipolar and hypothyroidism. Our THIN® analysis confirmed 13% of active patients with a diagnosis of bipolar disorder also have a diagnosis of hypothyroidism in THIN® (compared with just 3.4% of the general population) - 81% of these patients are female. Other associated conditions that are seen more often in women with bipolar than men include anxiety, migraines, obesity and panic disorders.
As a result it is advise that all people suffering from bipolar disorder should also be carefully screened for physical conditions such as thyroid imbalances, as well as heart diseases and diabetes.
Substance Abuse
Screening should also extend to include mental health complications, including substance abuse and anxiety disorders. While bipolar increases an individual’s risk of suicide by up to 20 times, it can take an average of ten and a half years to get a correct diagnosis of bipolar. Environmental factors may include stress, alcohol or substance abuse, and lack of sleep can have a notable effect on individuals with bipolar.
Our THIN® analysis confirmed the need to consider these factors:
- 31% of active patients with a diagnosis of bipolar disorder* have a reported history of self-harm in THIN®
- 38% of patients diagnosed with bipolar disorder* in 2019 have an alcohol measurement recorded in THIN® - and 19% of these reported drinking more than 14 units of alcohol a week (the NHS alcohol consumption recommendation)
This is where THIN can be so powerful in joining up the dots. Our data provides a clear representation of community and population health which, when combined with proactive strategies for improving population health, can deliver more effective models of care for patients.
Improving awareness and reducing stigma through World Bipolar Day is invaluable; but better understanding of the issues associated with day to day living with bipolar and the likely impact of highly stressful situations – such as the current coronavirus pandemic – are essential in helping people to get the right treatment and support.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.
*Patients with bipolar disorder were determined using read codes from Carr et al (2016) in combination with a prescription of the following drugs: lithium, lithium succinate, valproic acid, carbamazepine, lamotrigine, aripiprazole, olanzapine, quetiapine and risperidone