Coeliac Awareness Week
It takes on average 13 years from first symptoms to achieve a diagnosis of coeliac disease. Often confused with Irritable Bowel Syndrome (IBS), just 30% of people with coeliac disease are currently diagnosed according to Coeliac UK.
With an estimated half a million people in the UK living with undiagnosed coeliac disease, this year’s Coeliac Awareness Week, 11th -17th May, is encouraging individuals and clinicians to ask: ‘Is it Coeliac Disease?’.
Diagnosis Confusion
Coeliac disease is a common autoimmune disease caused by a reaction to gluten. Symptoms include diarrhoea, constipation, vomiting, stomach cramps, fatigue and anaemia. If undiagnosed, untreated coeliac disease raises the risk of complications including osteoporosis, neurological conditions such as gluten ataxia and neuropathy. Although rare, there is also an increased risk of small bowel cancer and intestinal lymphoma.
The wide range of symptoms associated with coeliac disease can create diagnostic confusion – symptoms can be confused with IBS or wheat intolerance, as well as stress and ageing. Indeed, one in four people with coeliac disease have previously been treated for IBS and been prescribed anticholinergics to relieve spasms, tricyclic antidepressants to relieve depression and severe pain, selective serotonin reuptake inhibitors (SSRIs) to relieve depression, pain and constipation, anticonvulsants for pain and bloating and anti-diarrhoeal drugs.
In contrast, once diagnosed, coeliac disease is treated by following a gluten free diet for life which is successful for the vast majority. For 5% of patients, damaged villi in the small intestine do not heal from a gluten free diet. These individuals suffer from Refractory Coeliac Disease (or Refractory Sprue) and are usually treated with steroids and immunosuppressants.
Time to Test
Coeliac disease in adults is diagnosed by serological testing and endoscopic intestinal biopsy. People with coeliac disease produce tissue transglutaminase antibodies (tTGA) and endomysial antibodies (EMA) when gluten is ingested. The National Institute for Health and Care Excellence (NICE) recommends the test for total immunological immunoglobin A (IgA) and IgA tissue transglutaminase (tTG) as a first choice. If IgA tTG is weakly positive, use IgA endomysial antibodies (EMA); also consider using IgG EMA, IgG deamidated gliadin peptide (DGP) or IgG iTG in cases of IgA deficiency. For these tests to produce valid results it is essential that patients continue with a gluten including diet before and during the diagnosis process, preferably including gluten in more than one meal a day for at least six weeks before testing.
Adults with a positive blood test and those with negative antibodies where coeliac disease is suspected should be referred to a gastroenterologist for a biopsy. Adding the biopsy to the diagnostic process is believed to be key in avoiding the repeated cycle of missed and delayed diagnosis, providing a cast iron diagnosis based on the density of intra-epithelial lymphocytes (IELs); crypt hyperplasia with a decreased villi/crypt ration; blunted or atrophic villi due to repeated gluten exposure; mononuclear cell infiltration in the lamina propria; epithelial changes, including structural abnormalities in epithelial cells.
In children, however, a biopsy is not recommended, as it is too invasive and requires a General Anaesthetic. The Total IgA and IgA tTG blood tests are recommended.
When to test?
The NICE guideline states that serological testing should be offered to children and adults presenting with persistent unexplained abdominal or gastrointestinal symptoms, faltering growth, prolonged fatigue, or unexpected weight loss. Additional flags include unexplained iron, vitamin B12 or folate deficiency, type 1 diabetes and autoimmune thyroid disease. It is also recommended that adults with IBS and first degree relatives of people with coeliac disease are tested.
In addition, there are number of other conditions that should prompt clinicians to consider coeliac disease, including metabolic bone disorder such as osteomalacia; unexplained neurological symptoms such as ataxia, unexplained subfertility or recurrent miscarriage and persistently raised liver enzymes with no known cause. Individuals with Down’s Syndrome and Turner syndrome are also known to be more susceptible to coeliac disease.
However, it is estimated that up to 30% of coeliac disease patients have persistent symptoms while on a gluten-free diet. While the most common reason for persistent symptoms is continuing to ingest gluten, it is also recognised that people with coeliac disease have an increased incidence of microscopic colitis and inflammatory bowel disease (Crohn’s disease and ulcerative colitis); as well as Small Intestinal Bacterial Overgrowth (SIBO) and Pancreatic Insufficiency.
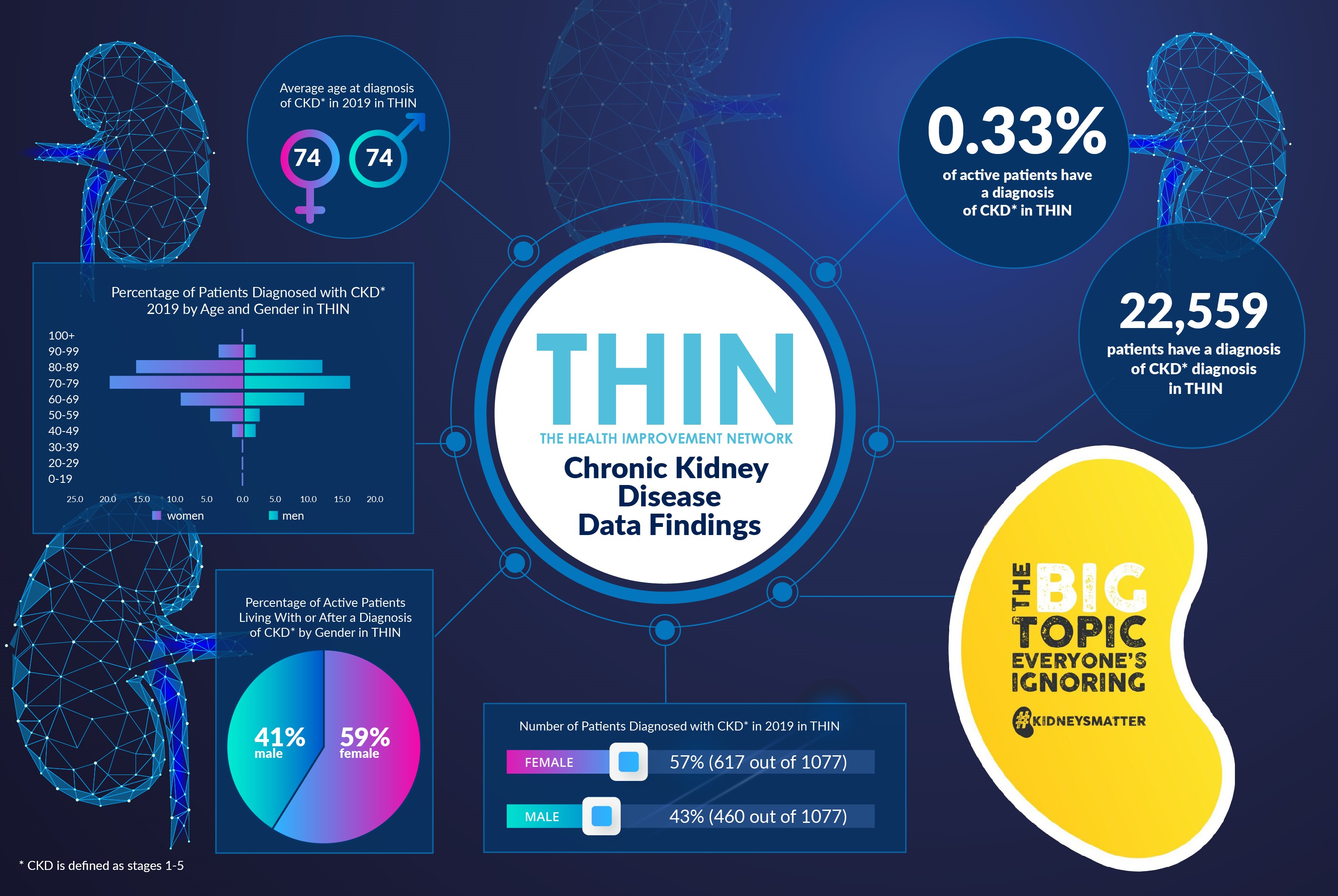
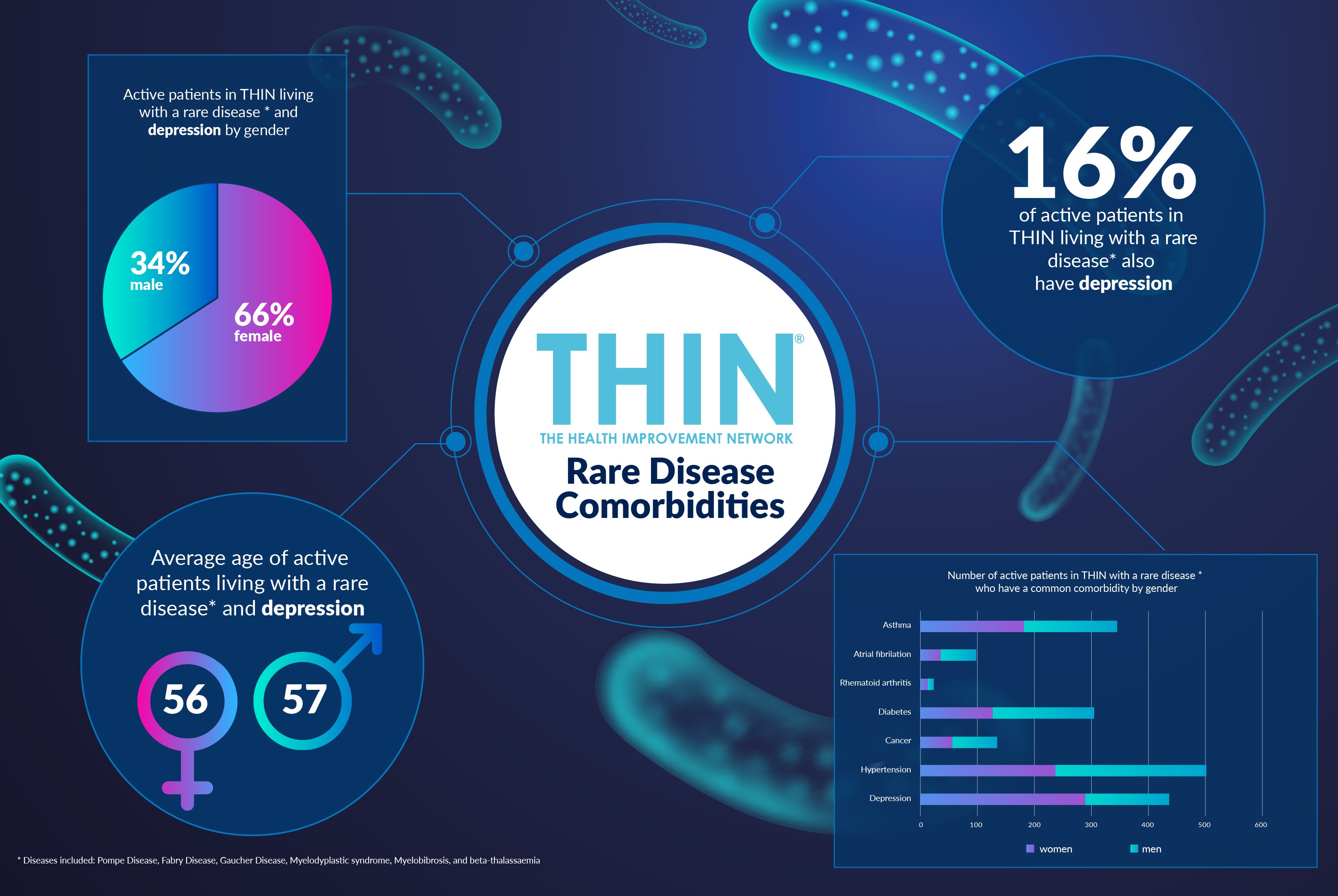
The diversity of symptoms and overlap with other potential conditions underlines the problems with diagnosis. This is where The Health Improvement Network (THIN®), a Cegedim Database, is so powerful. Providing direct access to anonymised longitudinal patient data, THIN® supports research into the patient pathway. By joining the dots and providing an in depth representation of community and population health, THIN® offers insight into the complexities of conditions such as coeliac disease, including those who have already been treated for IBS, treatment response and comorbidities, providing vital insight into this chronic condition.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.