Supporting Individuals Living with HIV/AIDS on World AIDS Day
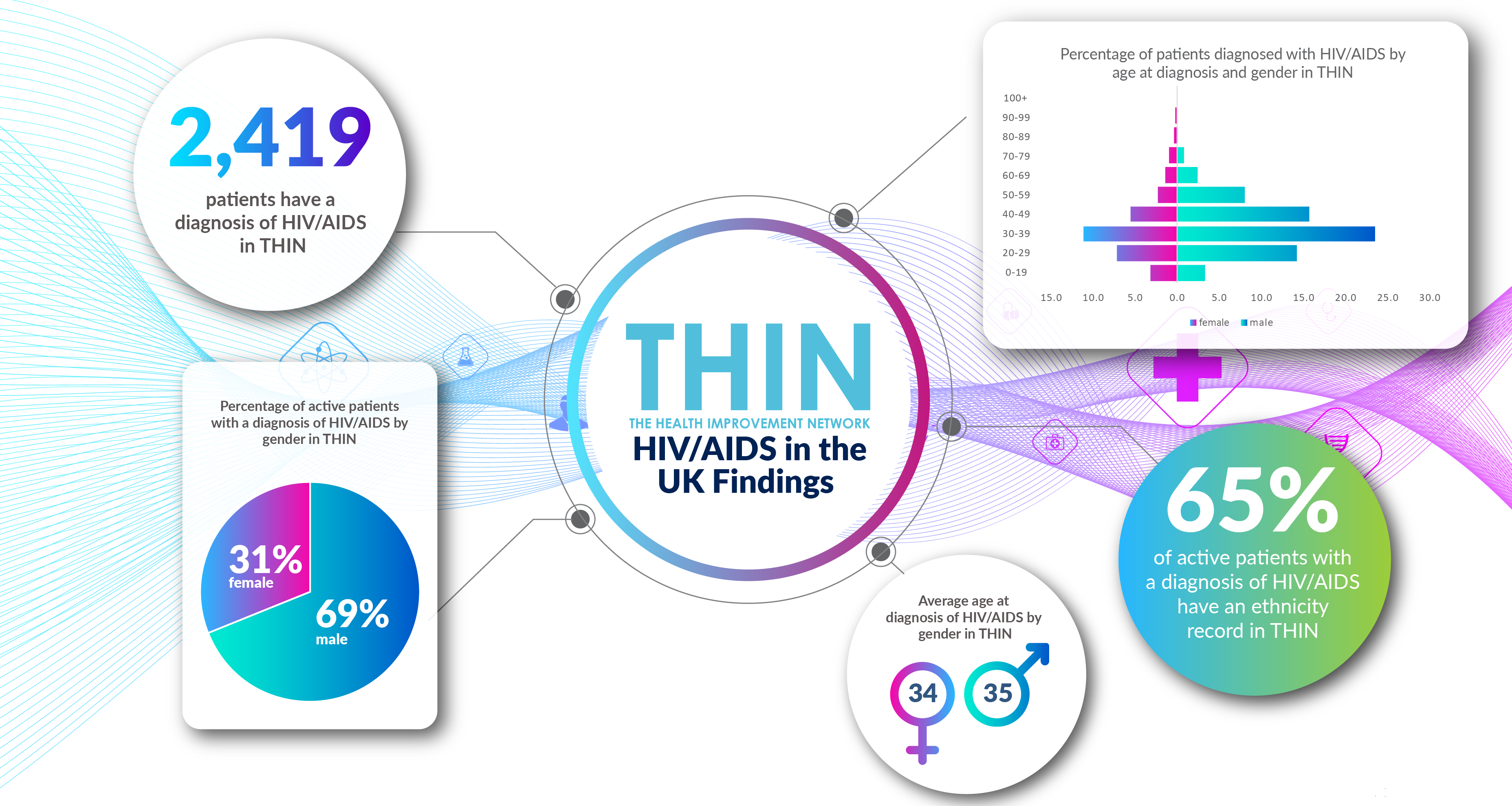
As the world comes together to fight one global pandemic, another still affects millions of people. Globally there are an estimated 38 million people living with HIV – over 100,000 in the UK. More than 35 million people have died of HIV (Human Immunodeficiency Virus) or AIDS (Acquired Immunity Deficiency Syndrome) since it was identified in 1984, making it one of the most destructive pandemics in history.
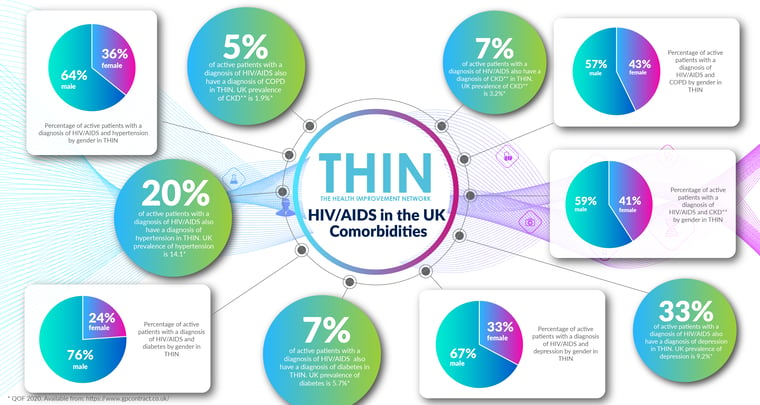
Since 2000, combined treatment regimes have significantly improved the outcomes for people with HIV – however, growing evidence of a rise in cardiovascular disease, hypertension, diabetes and chronic kidney disease within this population group reinforces the importance of proactively managing the health of individuals living with HIV.
World AIDS Day, on 1st December each year, is an opportunity for people worldwide to unite in the fight against HIV, to show support for people living with HIV, and to commemorate those who have died from an AIDS-related illness.
Virally Suppressed
COVID-19 may define the year 2020, but for many people the AIDS pandemic defined the 1980s. When the pandemic was first identified, transmission was not understood, and death was almost inevitable. Left untreated, HIV damages the immune system, reducing an individual’s CD4 count. AIDS is the most advanced stage of a HIV infection when the immune system can no longer fight infections.
Decades later and there have been huge scientific advances in HIV treatment: antiretroviral therapy (ART) does not cure HIV, but it stops the virus from reproducing in the body. It can reduce the amount of virus in the blood to undetectable levels, meaning that an individual cannot pass on HIV. Today, 97% of people diagnosed with HIV in the UK are on treatment, and 97% of those on treatment are virally suppressed.
However, despite improved understanding of the condition, over 4,450 people are diagnosed with HIV each year in the UK according to the National AIDS Trust. Furthermore, while it is estimated that 93% of those with HIV are diagnosed, one in 14 people living with HIV in the UK do not know that they have the virus. People still do not know how to protect themselves and others, and stigma and discrimination remain a reality for many people living with the condition.
Potentially Missed Diagnosis
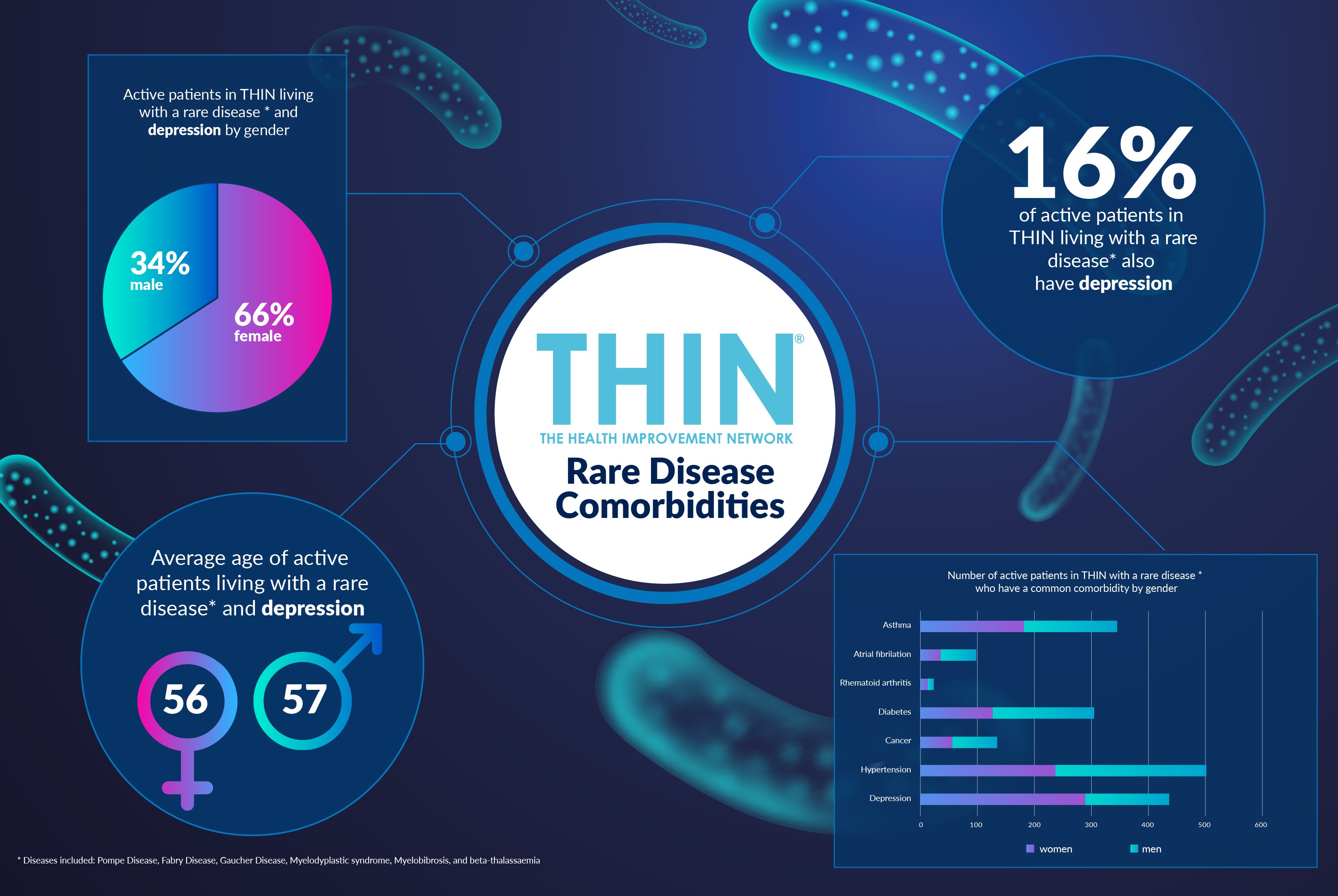
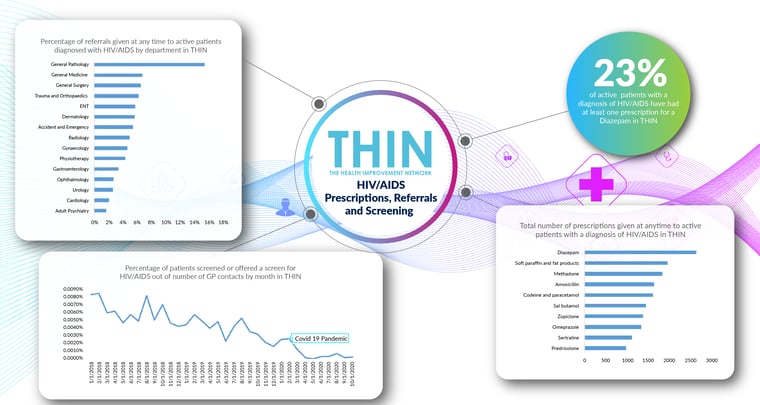
The prevalence of undiagnosed HIV is a particular concern given the lack of interaction with clinical care services during the COVID-19 pandemic. Analysis of data from The Health Improvement Network (THIN®), a Cegedim database, confirms that the percentage of patients screened or offered a screen for HIV/AIDS out of number of GP contacts by month, fell to zero in several months during the pandemic.
THIN® is recognised to offer one of the most reliable and respected sources of primary care data in the world, with a rich data set providing huge value to healthcare organisations. Capturing clinical consultations in primary care, when coded, structured, anonymised and analysed at scale, this data provides valuable insight into both the experiences of patients living with a specific disease or condition and trends in diagnosis.
Cardiovascular Disease
Information captured at this crucial intersection between patient and doctor is particularly key given the rise in hypertension amongst people living with HIV. Since the year 2000, access to ART has increased to 16 million individuals globally and the HIV-related mortality rate has halved from an estimated two million deaths in 2005 to one million in 2016. However, during the same time period cardiovascular disease mortality rates more than doubled in people living with HIV. Hypertension—the leading risk factor for mortality worldwide—is a growing problem in HIV-infected adults; and studies suggest HIV-infected adults on ART have a higher prevalence of hypertension when compared with HIV-uninfected individuals.
These findings are confirmed by THIN® data - 20% of active patients with a diagnosis of HIV/AIDS also have a diagnosis of hypertension in THIN®, compared to the UK prevalence of hypertension of 14.1%. Diabetes is also a noted comorbidity, especially for those on protease inhibitors, with one study revealing that HIV-positive men on HIV meds were three times more likely to be diagnosed with diabetes over a four-year period, compared with HIV-negative men. The male bias associated with this comorbidity is confirmed by THIN® data: 7% of active patients with a diagnosis of HIV/AIDS also have a diagnosis of diabetes in THIN® (compared to the UK prevalence of diabetes of 5.7%), and men make up 76% of this group.
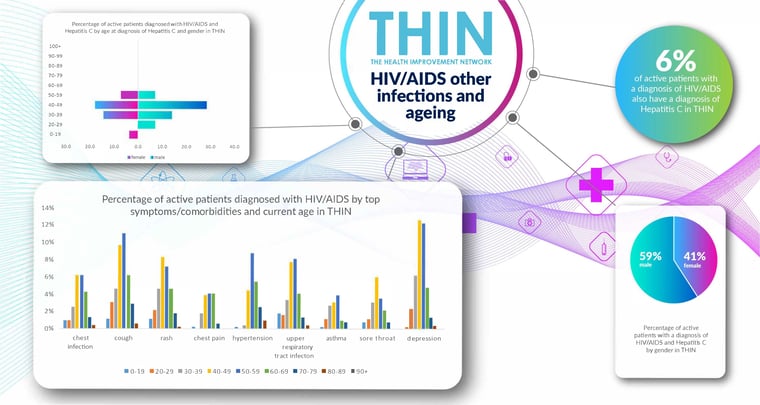
The impact of hypertension and diabetes on renal health is also underlined by THIN® data: 7% of active patients with a diagnosis of HIV/AIDS also have a diagnosis of Chronic Kidney Disease (CKD) in THIN®, compared to the UK prevalence of CKD of 3.2%. The Infectious Disease Society of America (IDSA) recommends that all people living with HIV be screened for kidney disease at diagnosis. Those at high risk for renal impairment—those with high blood pressure, diabetes, CD4 counts below 200, viral loads above 4,000 and hepatitis C co-infection—should be checked every year, even if they appear to have normal kidney function. THIN® data confirms that 6% of active patients with a diagnosis of HIV/AIDS also have a diagnosis of Hepatitis C.
Living Longer with HIV
The impact of ART is that many more individuals are living longer with HIV – with growing numbers of patients over 50. It is therefore even more important to understand the experience of those living with HIV, not only the incidence of cardiovascular disease but also mental wellbeing. THIN® data reveals that 33% of active patients with a diagnosis of HIV/AIDS also have a diagnosis of depression and 23% have had at least one prescription for a Diazepam, underling the importance of World AIDS Day in showing support for people living with HIV.
The use of epidemiological health data such as THIN® will play an important role in improving understanding of an ageing population living with HIV/AIDS as well as supporting policies for improving awareness to further reduce transmission levels.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.