Working Together on World Cancer Day
Cancer services have come under unprecedented pressure during the COVID-19 crisis – with recent analysis by the MacMillan Cancer Trust suggesting tens of thousands of people across the UK are missing a cancer diagnosis they would otherwise have received, because of the impact of the pandemic. The same problems are affecting cancer services globally: a survey conducted by the Union for International Cancer Control (UICC) with over 100 of its member organisations in 55 countries, including civil society, hospitals, research centres and patient support groups, revealed that their income and organisational activities are under significant pressure, with almost three-quarters reporting reductions in income of anywhere from 25% to 100% in 2020 and similar projections for 2021.
Cancer is a global challenge. In 2018, 18 million people world-wide were diagnosed with cancer. Today, thanks to research, one in two people in the UK survive their cancer for 10 years or more. The prospects of major advances in tackling cancer have never been greater, and international collaboration and funding are essential in realising these opportunities. This year’s World Cancer Day, on 4th February, is using the theme ‘I am and I will’ to reinforce the importance and power of cooperation and collective action.
Delays in cancer surgery are one of the biggest concerns facing NHS chiefs, as services struggle to cope with the impact of the pandemic, according to Sir Simon Stevens, the head of England's health service. He raised these concerns after figures reported by Health Service Journal suggested that there were 800 fewer cancer operations in the first two weeks of January, compared with the same time last year.
The impact of any delay in cancer treatment can be devasting - delaying cancer treatment by just four weeks increases the risk of death by up to 10%, according to new research that shows the devastating impact of missed NHS treatment targets due to Covid.
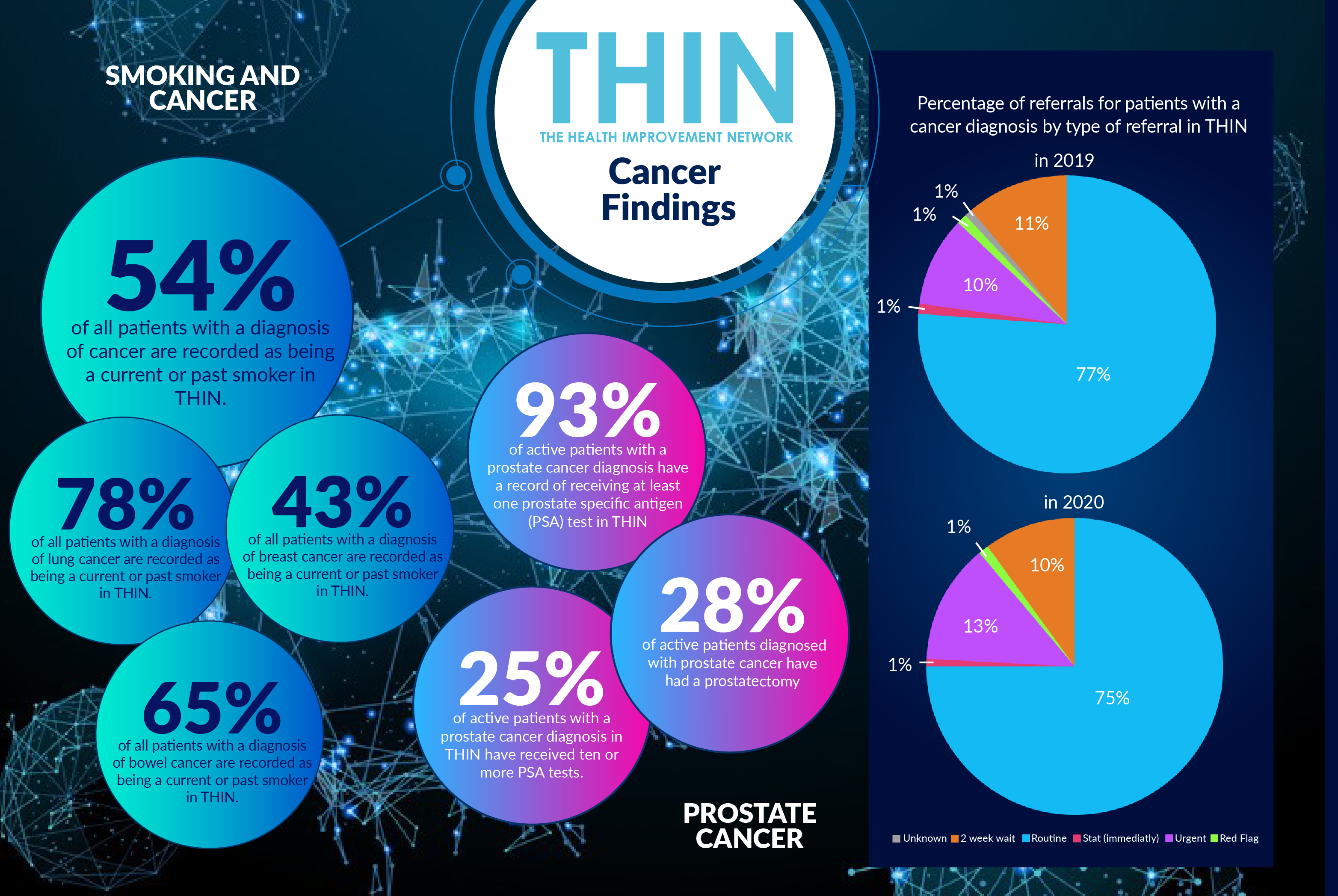
Analysis of The Health Improvement Network (THIN®), a Cegedim database, confirms that during 2020, the vast majority (75%) of referrals for active patients with diagnosed cancer were ‘routine. Just 9% of referrals were marked ‘two week wait’. However 13% were classified urgent, up from 10% the year before, 1% ‘red flag’ and 1% ‘immediate’.
Patient Concerns
Delays are now having a significant effect on patients, with new figures from MacMillan Cancer Trust revealing that cancer patients in the UK are now more worried about how delays to their treatment will impact on their chances of survival than they were following the first peak. More than a third (40%) of those receiving treatment in the UK in the run-up to the current lockdown — over 100,000 people — were worried that disruption caused by the coronavirus could be reducing the likelihood of their treatment being successful or, at worst, risk shortening their lives compared to around a quarter (28%) back in June.
So how can NHS services get diagnosis and treatment back on track? Better understanding of trends in diagnosis, testing and treatment is key to helping clinicians focus activity, which is where anonymised population health data such as THIN® can play a vital role.
THIN® has around 600,000 patients with a cancer diagnosis, and 85,000 active patients with a cancer diagnosis. The average age at diagnosis of cancer is 34 for men and 35 for women. For clinicians looking for insight to inform diagnosis, it is also interesting to understand the underlying lifestyle factors of patients with a diagnosis of cancer.
THIN® data also confirms the prevalence of smoking across cancers: 78% of patients with lung cancer, 65% of patients with a diagnosis of bowel cancer, and 43% of patients with breast cancer are recorded as being a past or current smoker in THIN®. In total, 54% of all patients with a diagnosis of cancer are recorded as being a current or past smoker in THIN®.
Testing Regimes
The NHS has different approaches to preventative testing for cancer – women are screened for cervical cancer every three years until the age of 50, and then every five years. Women over the age of 50 are also invited for routine breast screening every three years; while both men and women between the ages of 60 and 74 are invited to undertake a home bowel cancer screening test every two years. There is no screening for prostate cancer in the UK, due to concerns that the benefits may not outweigh the risks of this invasive procedure.
Analysis of THIN® data confirms that 93% of active patients with a prostate cancer diagnosis have a record of receiving at least one prostate specific antigen (PSA) test. In many cases, men are not advised to undergo invasive treatment immediately, with watchful waiting and active surveillance used to keep an eye on the cancer, and treatment only starting if it shows signs of progressing or causing symptoms.
Analysis of THIN® shows that a significant number of men are following this approach, with 25% of active patients with a prostate cancer diagnosis in THIN® having received ten or more PSA tests. However, 28% of active patients diagnosed with prostate cancer have had a prostatectomy – the surgical removal of the prostate gland in THIN®. This treatment has possible long term side effects, including an inability to get an erection and urinary incontinence.
Breast Cancer Treatment
THIN® also provides insight into the diagnostic and treatment experience for patients with breast cancer. Common breast cancer symptoms include lump in breast, breast soreness, mastodynia - pain in breast, breast mass, skin thickening of breast and induration of breast. Analysis of THIN® reveals breast lump symptom as the primary diagnostic factor (53%). 24% of active patients with a diagnosis of breast cancer had mastodynia, pain in the breast.
Moving to the treatment for breast cancer, including operations, biopsy and fine needle aspiration, 52% of active patients with a diagnosis of breast cancer have a record of having at least one breast procedure in THIN®. The vast majority of patients received a wide local excision of the breast lesion, a process which aims to remove benign and malignant lesions while conserving the normal shape of the breast as much as possible.
More Research is Needed
Studies have shown that radiotherapy after prostate removal surgery may increase the chances of a cure, but research is still being carried out into when it should be used after surgery. And it is the understanding of such treatment pathways that is key in improving patient outcomes in this challenging, pandemic dominated heath care environment.
On World Cancer Day, UICC is showcasing testimonies to illustrate how organisations and healthcare workers are rallying across the globe to support patients, resume screenings and diagnostics, maintain awareness on the need for prevention and provide a safe environment for treatment. Better understanding of population health data such as THIN® will continue to play a vital role in powering better pathways and creating safer, more effective models of care for patients.