Managing Allergy during and after the COVID-19 Pandemic
Allergy is the most common chronic disease in Europe. Currently affecting more than 150 million people, the EAACI predicts that by 2025 half of the entire EU population will suffer from chronic allergic diseases. Furthermore, up to 20% of patients with allergies struggle daily with the fear of a possible asthma attack, anaphylactic shock or even death from an allergic reaction.
The COVID-19 pandemic has been particularly challenging for those with allergies – from a lack of access to dedicated allergy clinics to problems locating substitutes for cows’ milk due to bulk buying and concerns regarding the use of oral steroids and other immunosuppressive tablets on immunity. In response, the World Allergy Organization has focused this year’s World Allergy Week (28th June to 4th July) on the theme: "Allergy care does not stop with COVID-19."
Understanding Allergy
BSACI defines allergy as a hypersensitivity reaction in which the immune system produces IgE antibodies against harmless antigens such as pollens, house dust mites, moulds, cat dander and foods. The IgE reaction to these allergens results in the release of chemicals including histamine as well as local or general inflammation and allergic response symptoms range from sneezing, wheezing, itching and rashes to anaphylaxis.
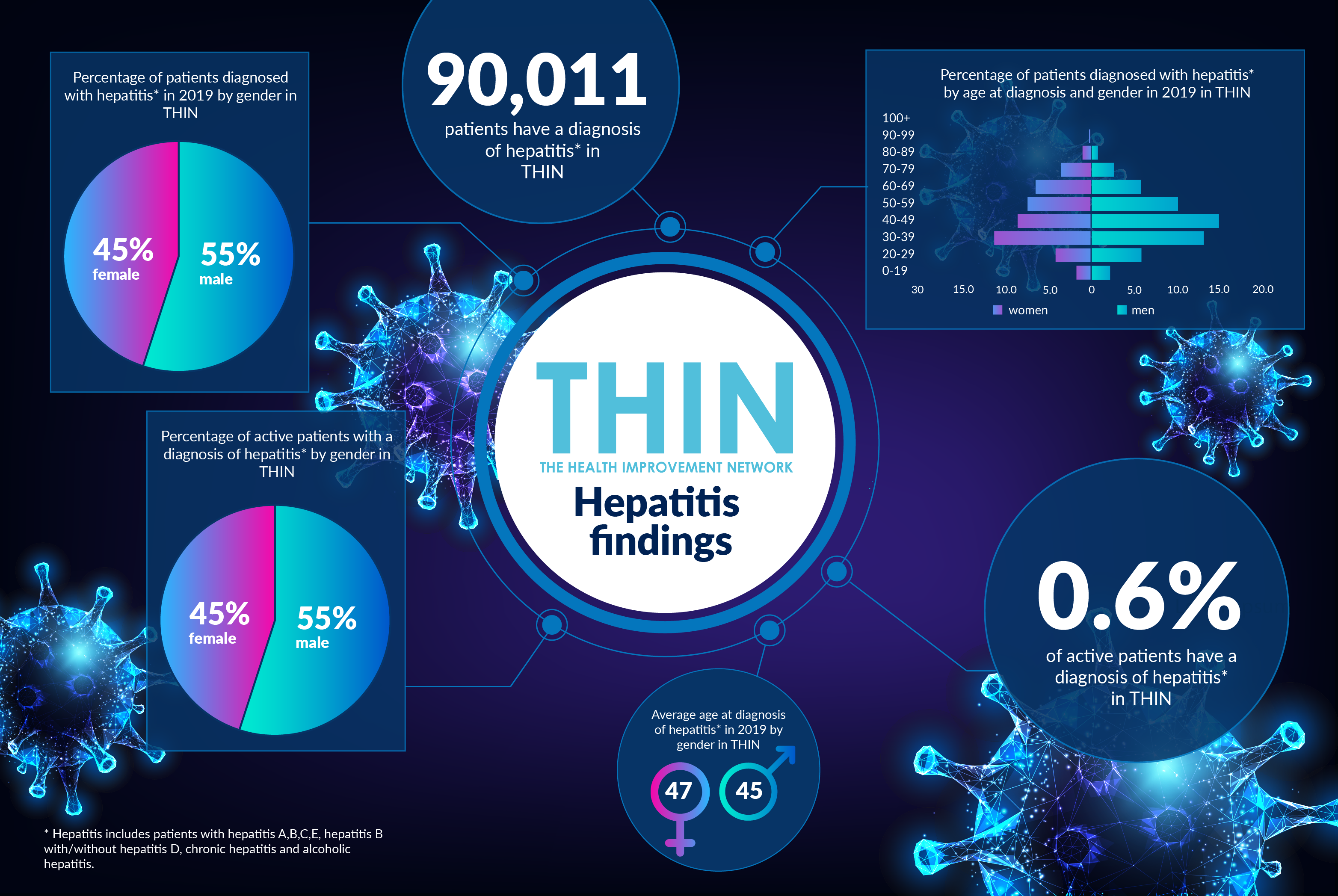
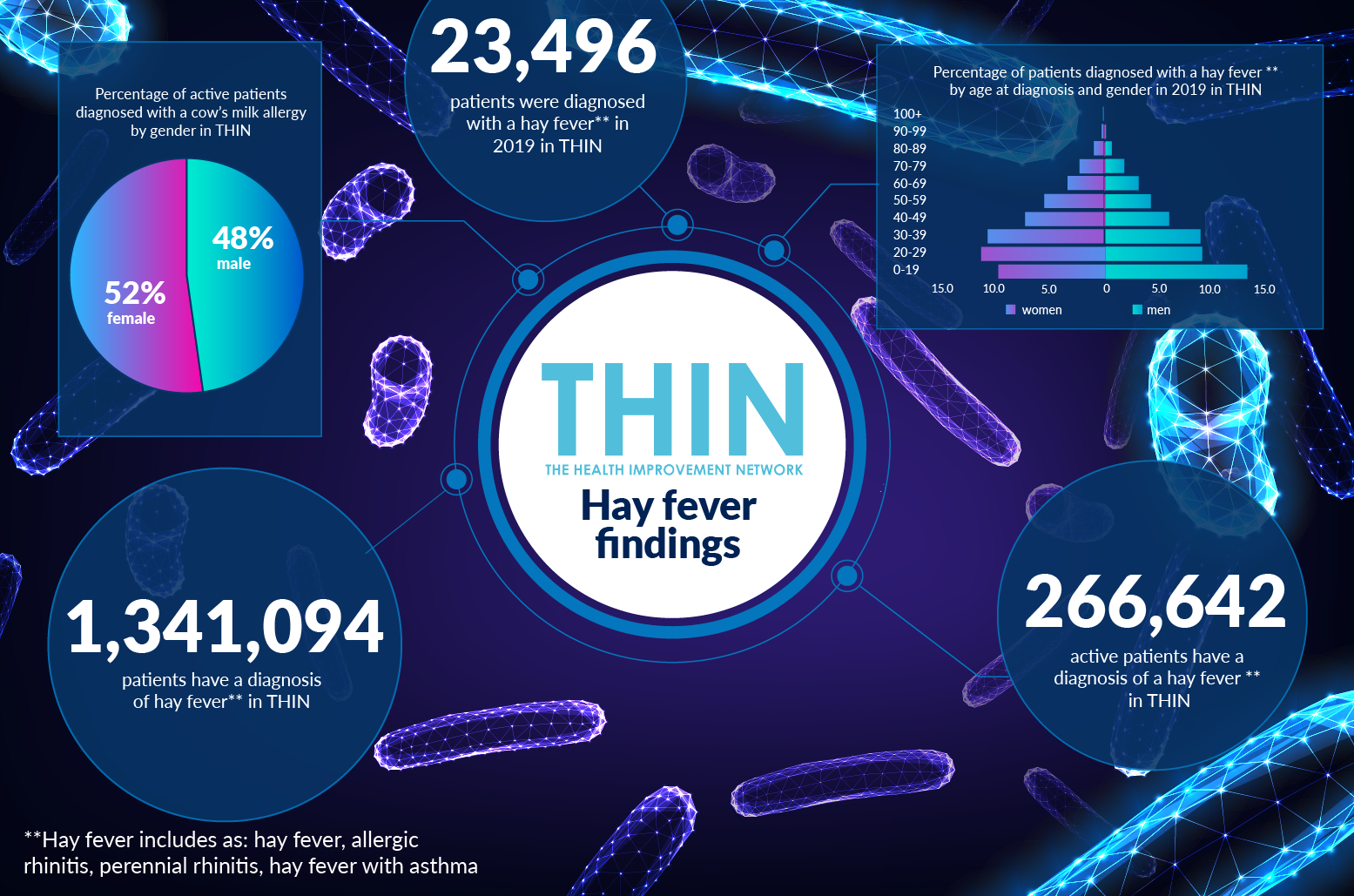
Both the incidence and severity of allergy in the UK are growing – 44% of British adults now suffer from at least one allergy and the number of sufferers is on the rise[1]; while in the 20 years to 2012 there was a 615% increase in the rate of hospital admissions for anaphylaxis in the UK[2]. This rise in allergy is reflected by data within The Health Improvement Network (THIN®), A Cegedim Database, which confirms that 114,315 patients have a diagnosis of a food allergy* in THIN®, while 1,341,094 patients have a diagnosis of hay fever.**
Allergy in Children
The incidence of allergy in children is a particular concern. The bulk of allergic disease occurs in childhood, with asthma, allergic rhinitis, and eczema and food allergy comprising a significant percentage of the workload of doctors dealing with children in primary care and hospital paediatric departments. A recent UK survey revealed a three-fold increase in prevalence of allergy compared with similar studies in the 1970s – and almost half (47%) of these children had at least two co-existing condition, such as asthma and eczema.
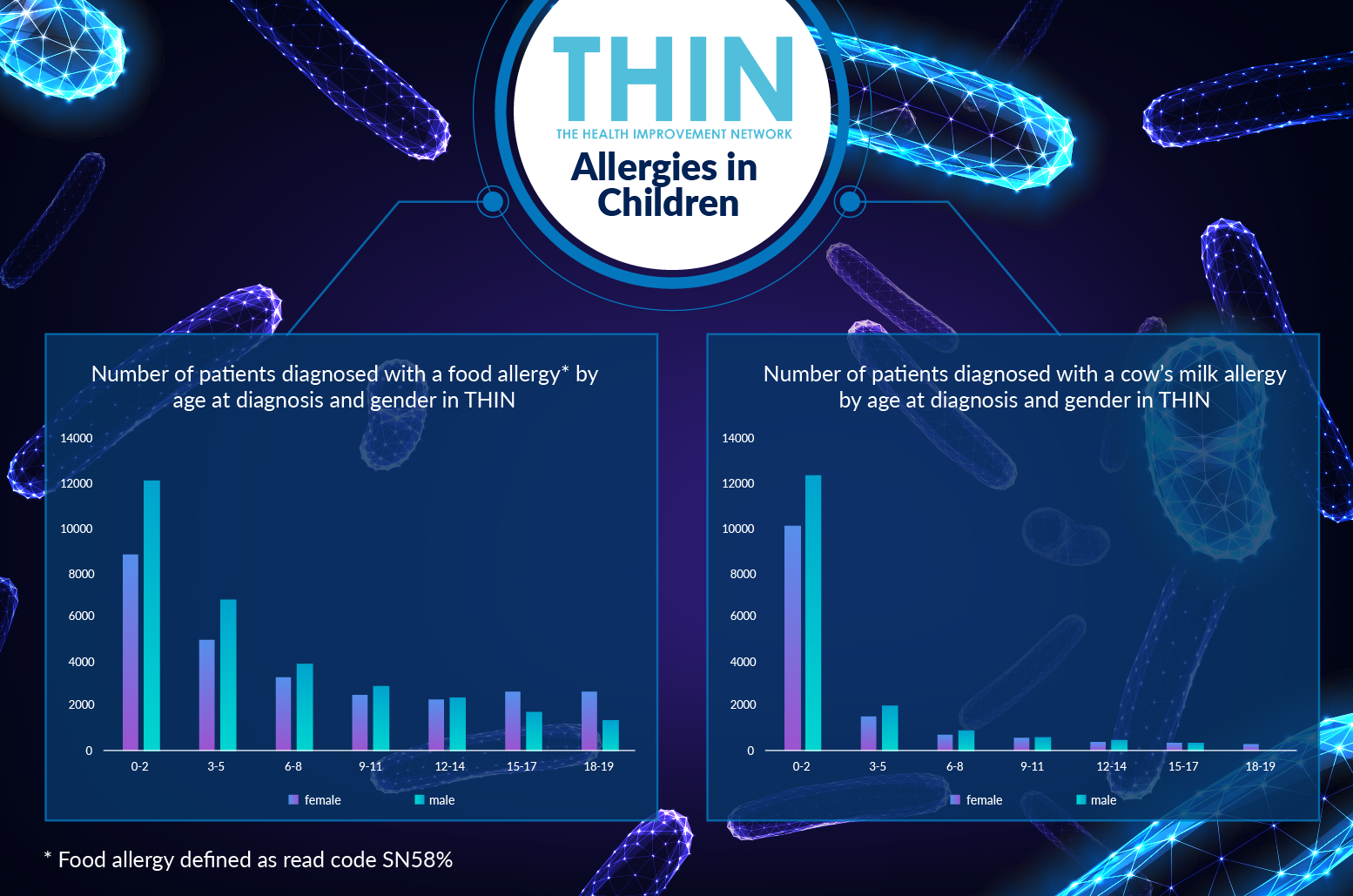
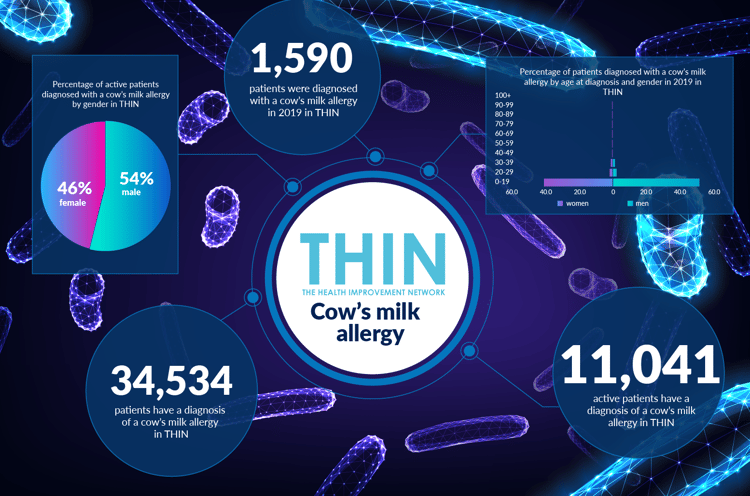
The rise in childhood allergy is confirmed by analysis of THIN® data, which reveals that almost half (49%) of patients are with food allergy are diagnosed under the age of 20. The figures are even more striking for allergy to cow’s milk: 34,534 patients have a diagnosis of a cow’s milk allergy in THIN® and 91% received that diagnosis before the age of 20. Furthermore, 54,928 patients have received a prescription for a cow’s milk substitute *** in THIN® and in 99.5% of cases patients received their first prescription for a cow’s milk substitute under the age of 20.
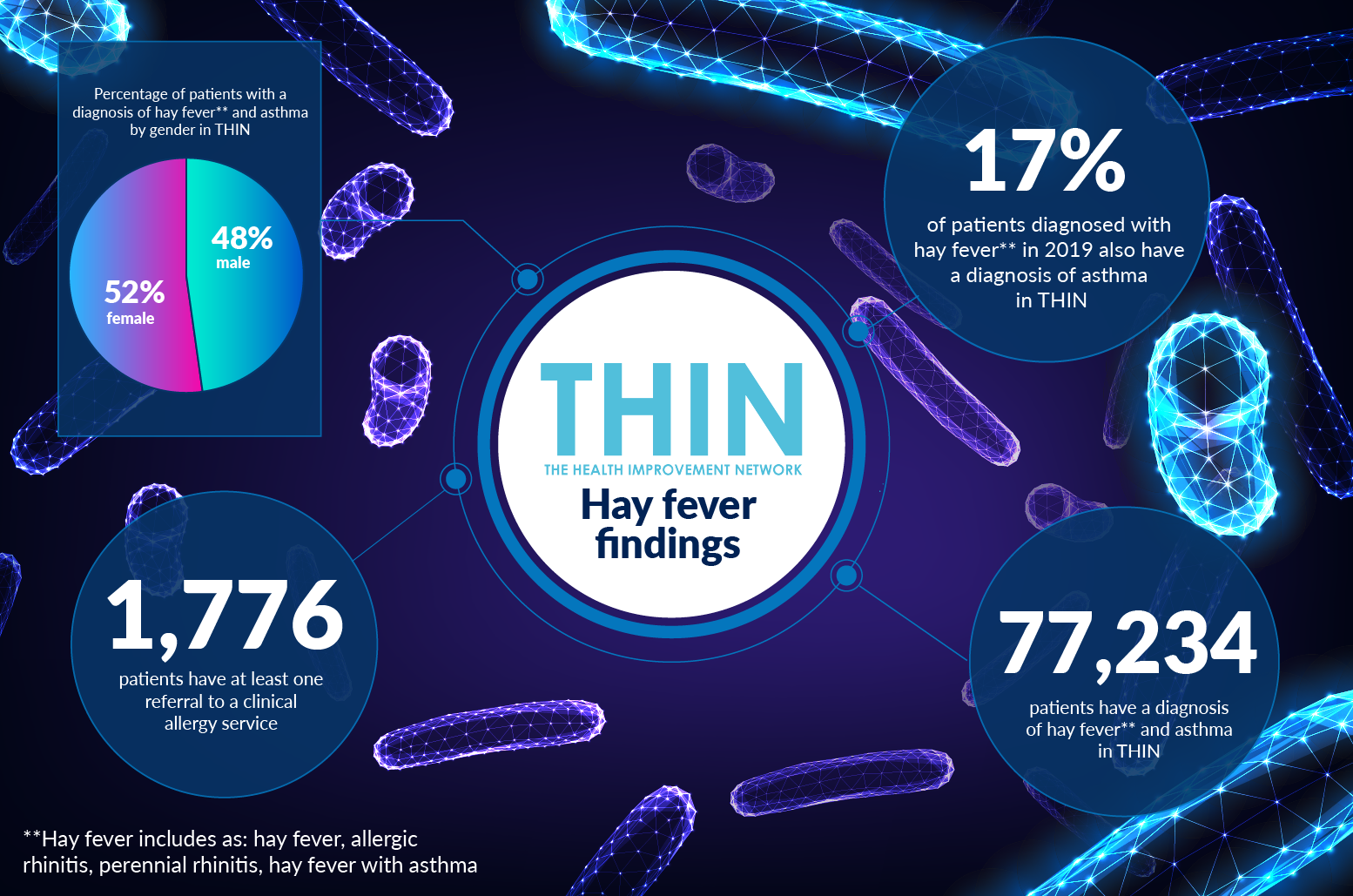
Hay Fever (allergic rhinitis) is the most common form of non-infectious rhinitis, affecting as many as 30% of adults and 40% of children[3]. The prevalence of more than one chronic allergy is also revealed by THIN® analysis: 17% of patients diagnosed with hay fever in 2019 also have a diagnosis of asthma; indeed a total of 77,234 patients have a diagnosis of hay fever and asthma in THIN®.
Managing Allergy
The severity of allergy is also underlined by THIN® data which reveals 20,732 patients have a record of anaphylaxis. It is also interesting to note that while allergies generally affect both sexes equally, women are more likely to experience anaphylaxis: 57% of patients with a record of anaphylaxis in THIN® are female. Women, as a result, also receive more prescriptions for epinephrine – the treatment for anaphylaxis: 82,417 patients have received a prescription for epinephrine in THIN® (56% to female patients). In addition, 235,118 patients received a prescription for antihistamine in 2019 - 61% of these were prescribed to female patients.
Given the rise in both number and severity of allergy throughout the UK, it is interesting to note that just 1,776 of patients within THIN® have received a referral to a clinical allergy service. With patient waiting lists increasing as a result of the pandemic, it will be important to understand how patients with allergy – especially the growing number of children – are able to manage the condition. The use of epidemiological health data such as THIN® to track the rise in allergy as well as monitor the outcomes for these individuals will be key to understanding how allergy is supported post COVID-19.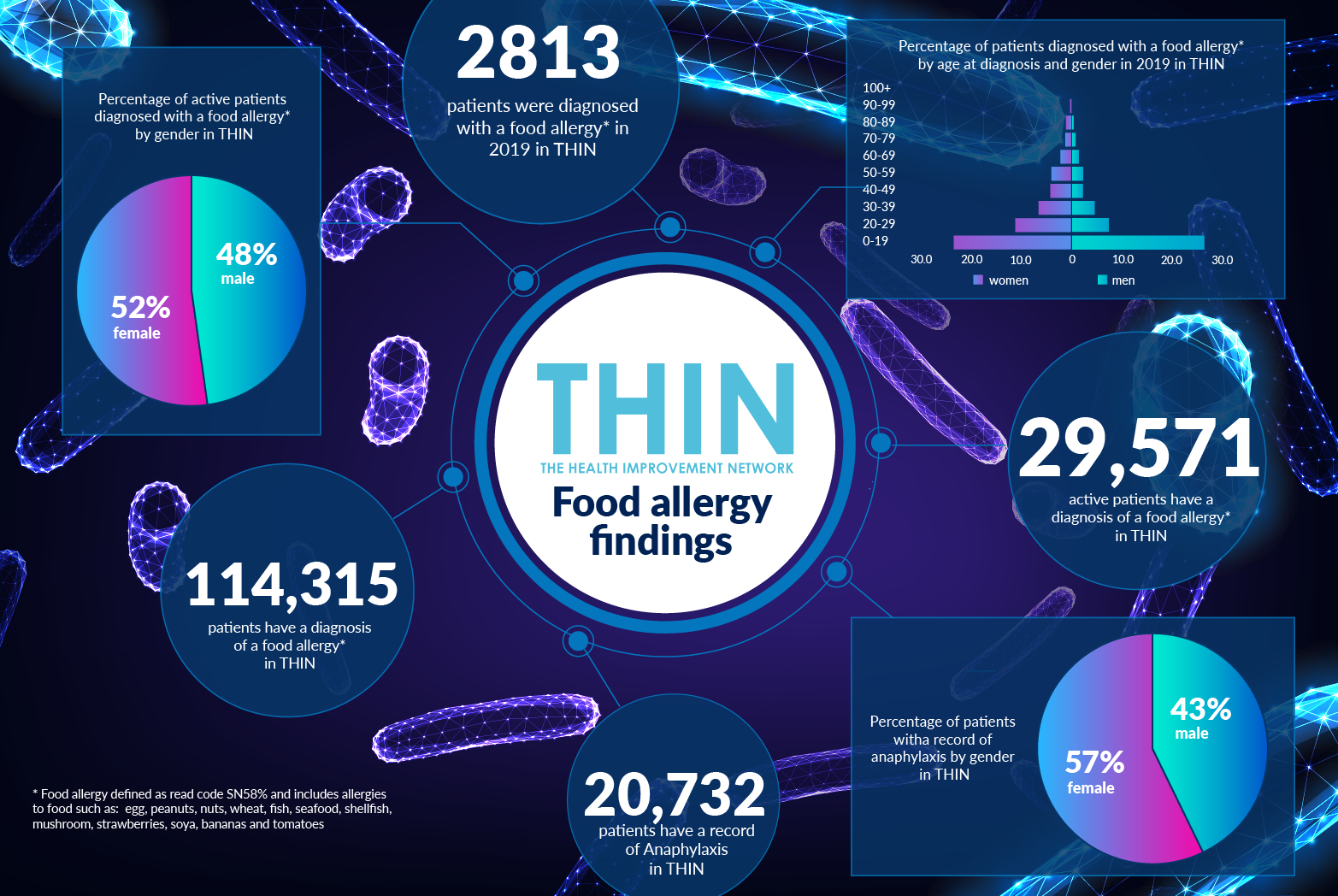
[1] Mintel, 2010
[2] Turner, Paul J., et al, 2015
[3] Pawankar R, et al, 2013
* Food allergy defined as read code SN58% and includes allergies to food such as: egg, peanuts, nuts, wheat, fish, seafood, shellfish, mushroom, strawberries, soya, bananas and tomatoes
**Hay fever includes as: hay fever, allergic rhinitis, perennial rhinitis, hay fever with asthma
*** Cow’s milk substitute defined as the following: Aptimal Pepti, Nutramigen, Similac Aliementum, Neocate, Alfamino and Nestle Althere.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.