Understanding the causes of obesity is key to prevention

The danger of obesity has come in to sharp relief during the past year, with obesity cited as a key COVID-19 comorbidity. A report from Public Health England concluded that a BMI of 35 to 40 (obese) may increase the risk of death from COVID-19 by 40%, while a BMI of over 40 (morbidly obese) could increase the risk by 90%.
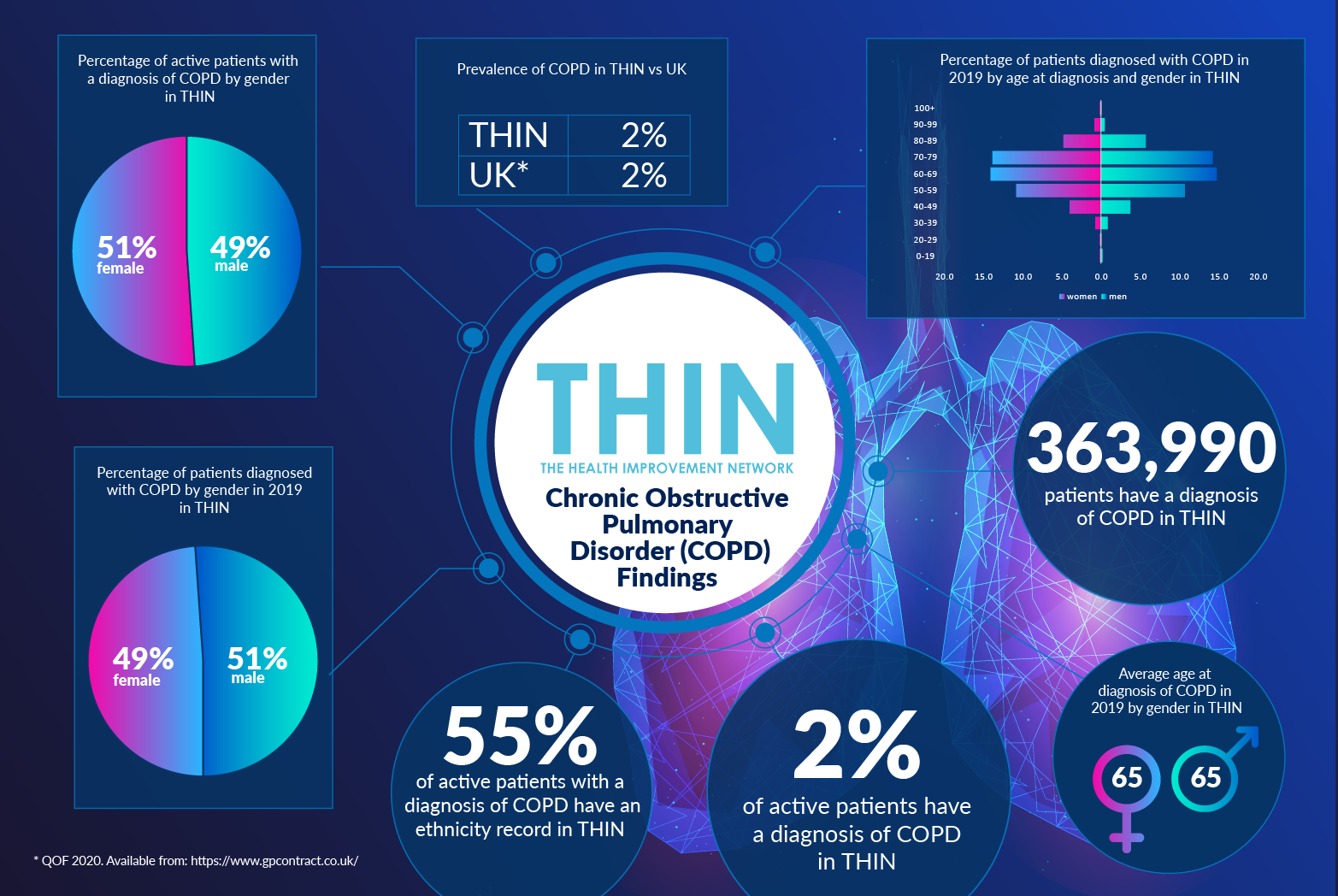
But the issues associated with obesity extend far beyond the pandemic. The comorbidities associated with obesity, including type II diabetes and chronic obstructive pulmonary disease (COPD), can have a life limiting impact. Furthermore, given the increasing pressure on the health care services, the continued rise in obesity, not only in the UK but throughout the world, is serious.
National Obesity Week aims to tackle the issue by reminding us all about the difficulties that come from being obese, what we can do to prevent it and how we can correct it if we are affected.
Rapidly escalating health problem
With more than 1 out of every 4 UK adults now classified as very overweight or obese, weight is now a national health issue. It’s thought that by 2035 the rates of severe obesity across the whole UK population will be double that of the current rate. Many healthcare practitioners are concerned about not only the health risks associated with obesity, but by the pressure this could put on the NHS.
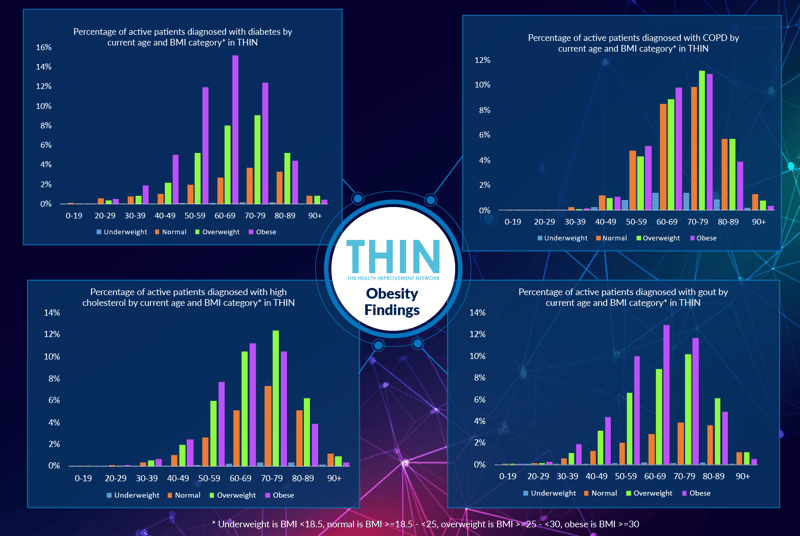
And for very good reasons. As analysis of The Health Improvement Network (THIN®), a Cegedim database, reveals, overweight and obese individuals experience many health complications, including type II diabetes, coronary heart disease, high cholesterol and gout. Excess weight is also associated with psychological conditions including low self-esteem, anxiety and depression.
Population Health
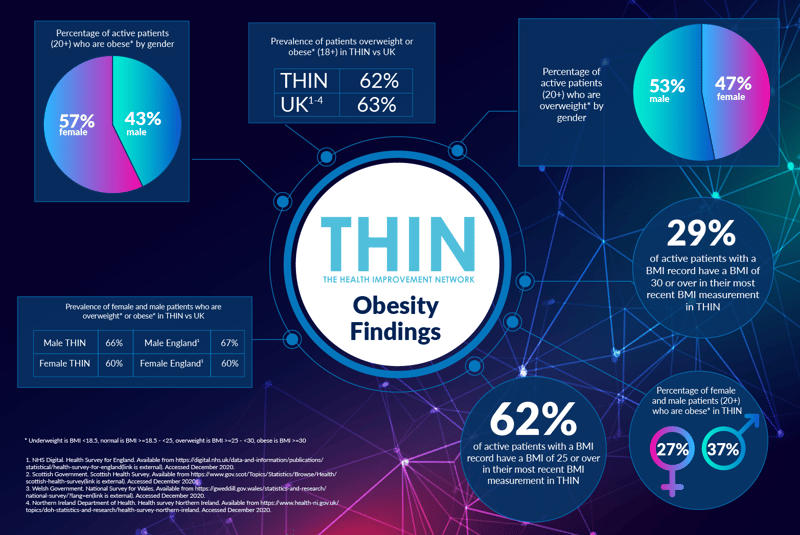
To better understand both the increase in obesity and the health implications, it is to analyse how obesity affects the population. Men are more likely to be overweight than women; however, levels of obesity are higher in women – 57% of obese individuals in THIN® are female.
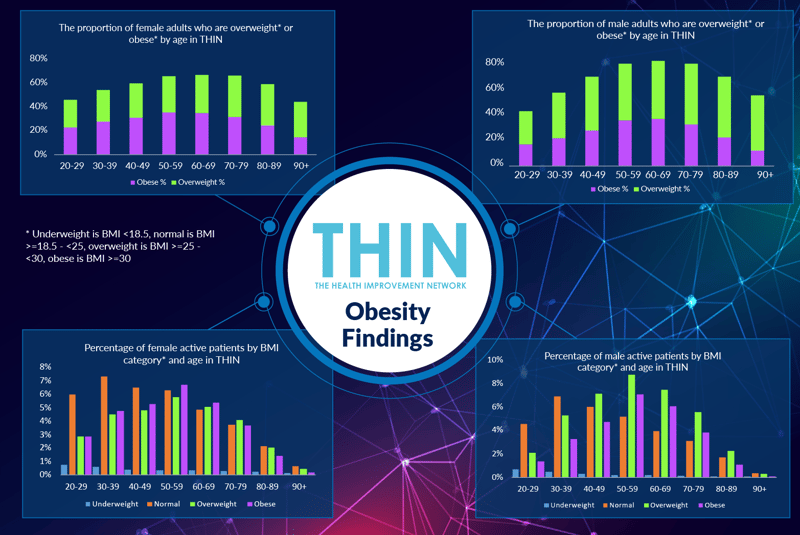
Individuals put on weight decade by decade through to their seventies at which point the proportion of overweight individuals starts to decline – although this could be due to higher morbidity. Between the ages of 60 and 69, two thirds (66%) of women are either overweight (32%) or obese (34%); while three quarters (76%) of men the same age are either overweight (42%) or obese (34%).
Obesity prevalence increased steeply between 1993 and 2000, according to the NHS, with a slower rate of increase since that date. The health implications and demands on NHS resources cannot be ignored: one quarter (26%) of individual with a diagnosis of high cholesterol in THIN® are aged 60-69 – and of those 80% are either overweight (38%) or obese (43%). The health implications of obesity can be seen in many areas, including a higher incidence of gout, diabetes and COPD.
Obesity Prevention
The COVID-19 comorbidity has prompted the UK government to announce a new obesity strategy for England, which includes a ban on television and online advertisements for food high in fat, sugar, and salt before 9 pm, calorie content displayed on restaurant menus for food and alcoholic drinks, and an end to “buy one and get one free” deals on unhealthy food.
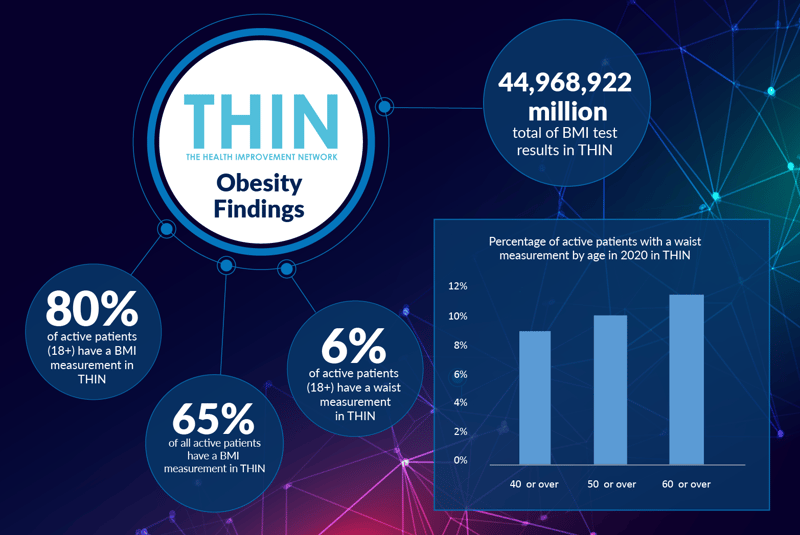
NHS weight management services will be expanded to reach more people, and GPs will be encouraged to prescribe exercise and more social activities to help people keep fit as part of the plans. GPs rely heavily on the use of BMI records to track patient progress - indeed, analysis of THIN® data reveals a total of 44,968,922 million BMI test results in THIN®.
Effective weight management requires repeated measurement – and the THIN® data reveals more than 10.6 million BMI records for more than 1.6 million active patients aged 18+ in THIN®. Over two thirds (68%) of active male patients aged 18 and over have more than one BMI record, rising to over four fifths (83%) of active female patients. In total, on average active patients have between six and seven BMI records each in THIN®. This repeated tracking of patients’ BMI that can provide better insight into the success of different weight management regimes, as well as the associated implications for patient wellbeing.
Waist to Height
There is also growing focus within the healthcare community on the value of the waist to height ratio (WHtR) as an alternative or addition to BMI data which cannot differentiate between fat and muscle – a fact that will lead many fit athletes to recording high BMIs. WHtR is a better indicator of an individual’s body fat distribution which can be a significant early indicator of risk of diabetes heart disease and stroke.
NHS advice suggests individuals should lose weight if they have a waist measurement of 94cm (37 inches) or more for men, and 80 cm (31.5 inches) or more for women. Individuals are also deemed to be at very high risk of serious health conditions if they have a waist measure of 102 cm (40 inches) or more in men, and 88 cm (34.5 inches) or more for women.
The WHrT ratio figures are simple – essentially an individual’s waist should measure no more than half the length of their height. For a 6ft man (72 inches), this means having a waistline no larger than 36 inches, while a 5ft 4in (64 inch) woman’s waist should measure 32in or less. For people under the age of 40, a WHtR of over 0.50 is considered to put them at critical risk. For the over fifties the critical values start at 0.60.
Proactive Support and Management
Patients’ waist measures should be routinely checked during the over 40 and 50 NHS health checks – and using tools such as Cegedim’s Outcomes Manager, will prompt for this measure and automatically calculate the WHtR figure. However, analysis of THIN® data confirms that only 9% of active patients 40 or over, 10% of active patients 50 or over and 11% of active patients 60 or over in THIN® have a waist measurement.
Evidence is growing regarding WHtR’s value as an effective indicator of early health risk, reinforcing the value of deep longitudinal data sources such as THIN® both in understanding the health implications of obesity and providing the insight to create supportive and effective weight management plans.