Prioritising COPD Care During Peak Hospitalisation Season
Life with chronic obstructive pulmonary disease (COPD) can be difficult. It is a progressive condition, there is no cure and everyday tasks can become a challenge. As we head into winter – the deadliest time for people with lung conditions – there is rising concern regarding the dual implications of contracting COVID-19 and the acknowledged backlog in basic care that has occurred over recent months.
COPD describes a group of conditions that cause narrowing of the lungs, making it difficult to empty air from the lungs. The conditions, including long-term (or chronic) bronchitis and emphysema, usually develop due to long-term lung damage caused by breathing harmful substances. Cigarette smoke is a primary cause, as is air pollution – although jobs that expose individuals to dust, fumes and chemicals can also contribute to developing COPD.
On World COPD awareness day on November 18th the focus is on helping individuals to better manage the condition.
Winter Challenge
The winter months are always challenging for individuals with COPD – plummeting temperatures, colds and flu cause symptoms to flare up and trigger potentially life-threatening exacerbations. There are 80% more lung disease admissions in the winter months of December, January and February than in the warmer spring months of March, April and May. This year, we have to add COVID-19 to the risk factors – not on the devastating potential impact of catching the virus but also the delays in care that have occurred since March 2020.
The Taskforce for Lung Health is calling for people with suspected or diagnosed chronic obstructive pulmonary disease to receive more support during and after the pandemic. Asthma UK and the British Lung Foundation estimates that up to 1.8 million people with lung conditions could have missed out on annual reviews during lockdown, essential for helping people stay on top of symptoms and ensuring they are on the correct medication.
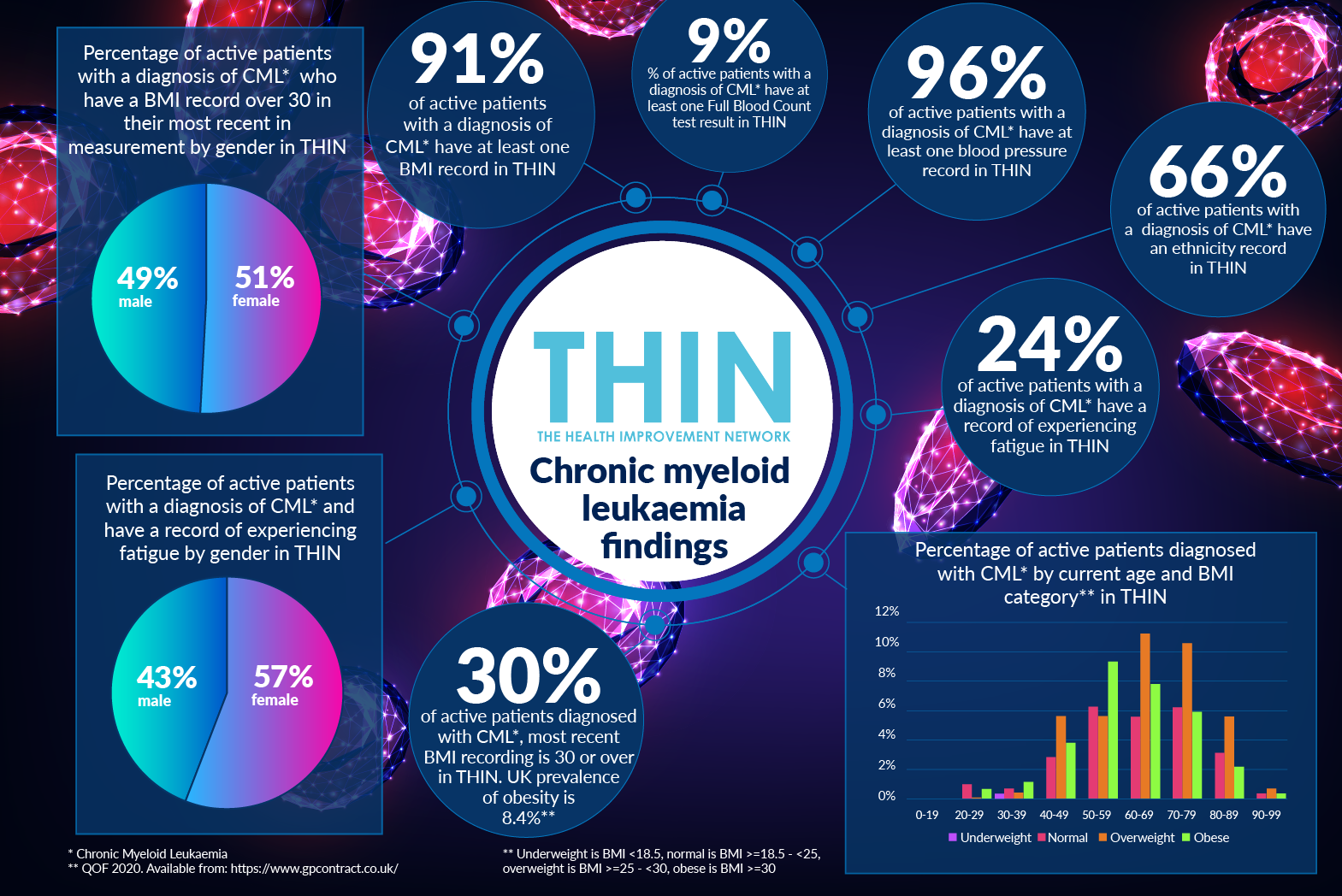
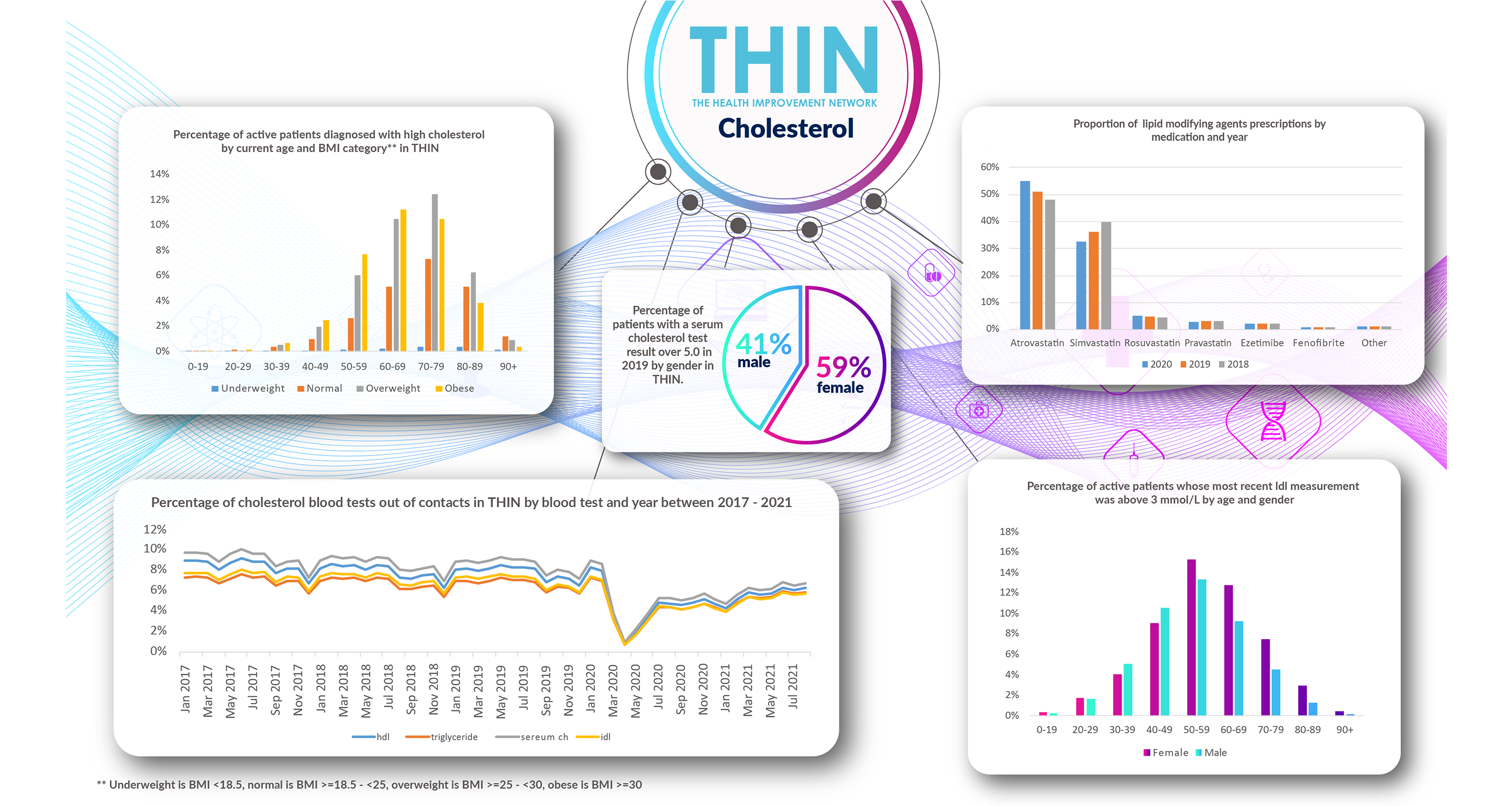
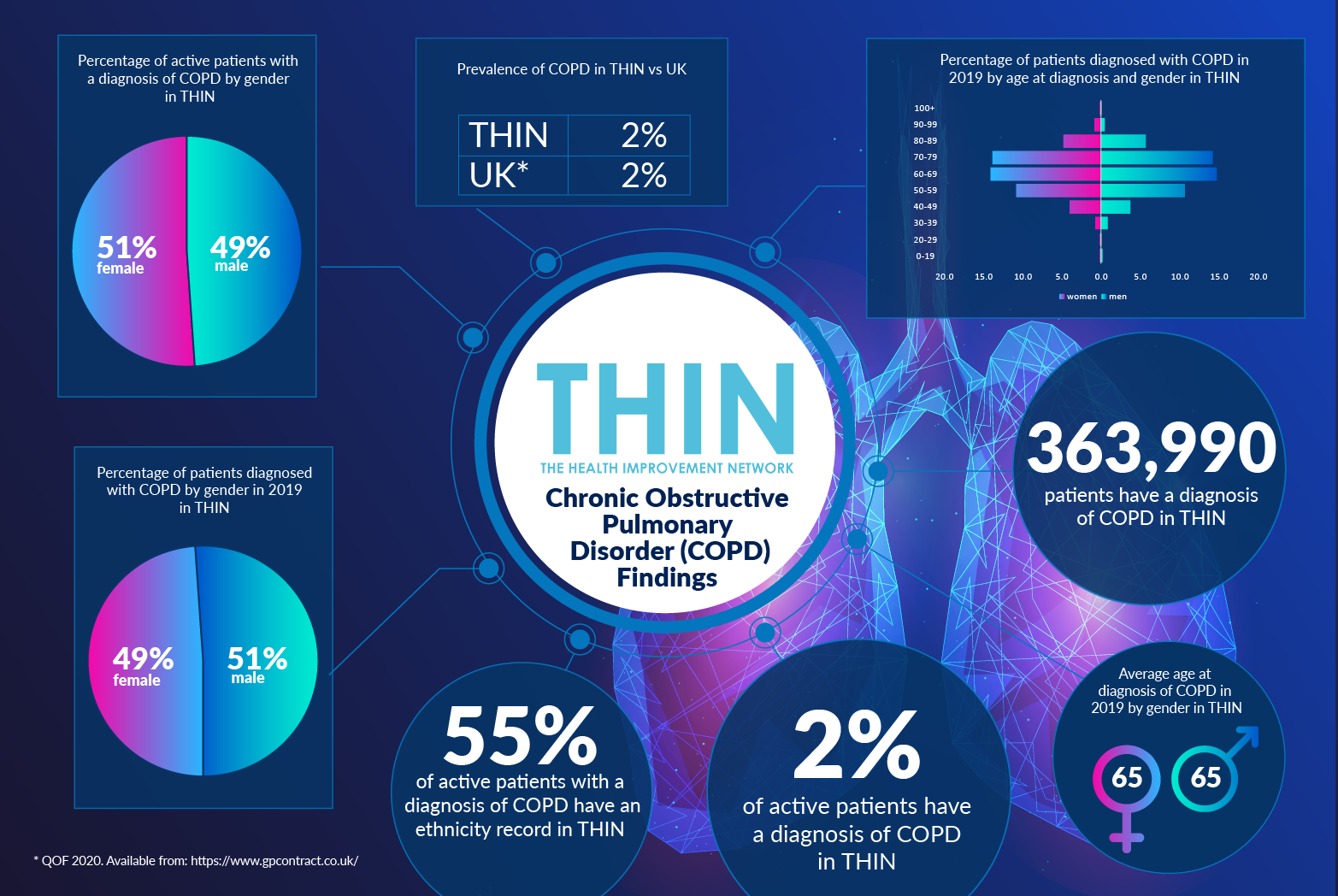
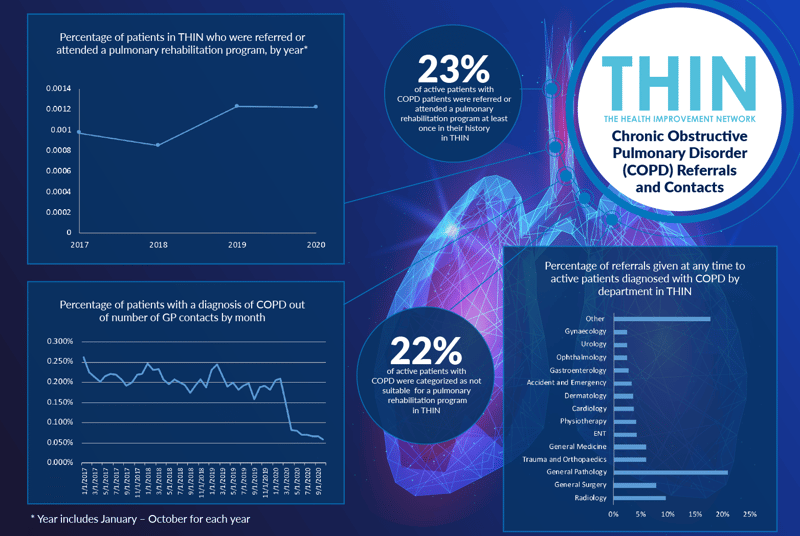
Concerns regarding the lack of clinical interaction during the pandemic are verified by analysis of The Health Improvement Network (THIN®), a Cegedim Database. Between March and September 2020, the percentage of GP contacts of patients with a diagnosis of COPD plummeted to a quarter of usual levels.
Managing Complex Health Needs
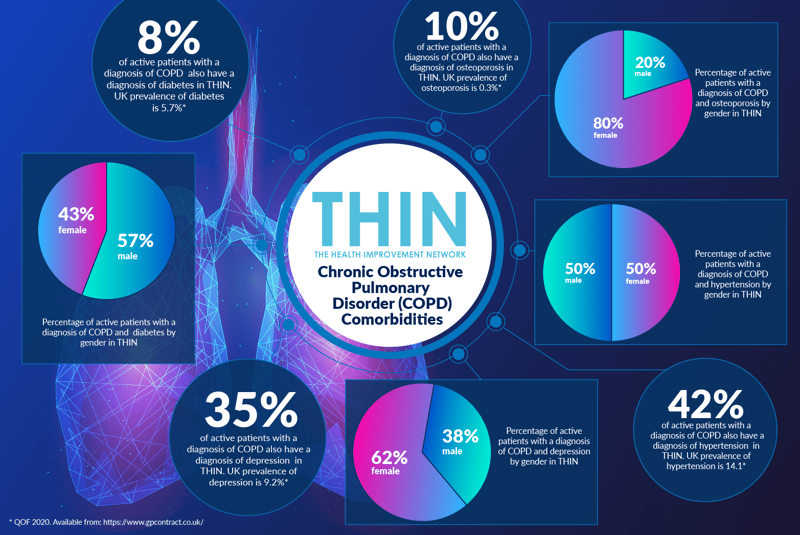
The issue is not simply managing COPD – many individuals have complex health needs with one or more comorbidities. 42% of active patients with a diagnosis of COPD also have a diagnosis of hypertension in THIN® – compared with a UK prevalence of hypertension of 14.1%. Diabetes is also a factor - 8% of active patients with a diagnosis of COPD also have a diagnosis of diabetes in THIN®, compared to the UK prevalence of diabetes of 5.7%.
Diabetes is more likely to affect men (57%) with an active diagnosis of COPD than women – while women with COPD are more likely to also suffer from depression and osteoporosis. Over a third (35%) of active patients with a diagnosis of COPD also have a diagnosis of depression in THIN®, compared to the UK prevalence of depression at 9.2%. Almost two thirds (62%) are women. 10% of active patients with a diagnosis of COPD also have a diagnosis of osteoporosis in THIN® – compared to the UK prevalence of osteoporosis at 0.3% - 80% of these individuals are women.
Reduced lung capacity will often restrict an individual’s day to day activity, having clear implications on weight as well as strength and mental health. This is one of the reasons that prevention and care strategies are such an important part of the management of COPD.
Care and Prevention
Pulmonary rehabilitation is a key component of COPD care and support. The six to eight week treatment programme includes both a tailored physical exercise programme and information to help individuals manage COPD day to day. The programme addresses not only lung function but also strength and mental well-being. However, according to THIN® data, less than a quarter (23%) of active COPD patients have been referred to attended pulmonary rehabilitation programme at least once in their history in THIN®. 22% of active patients were categorised as not suitable for the programme.
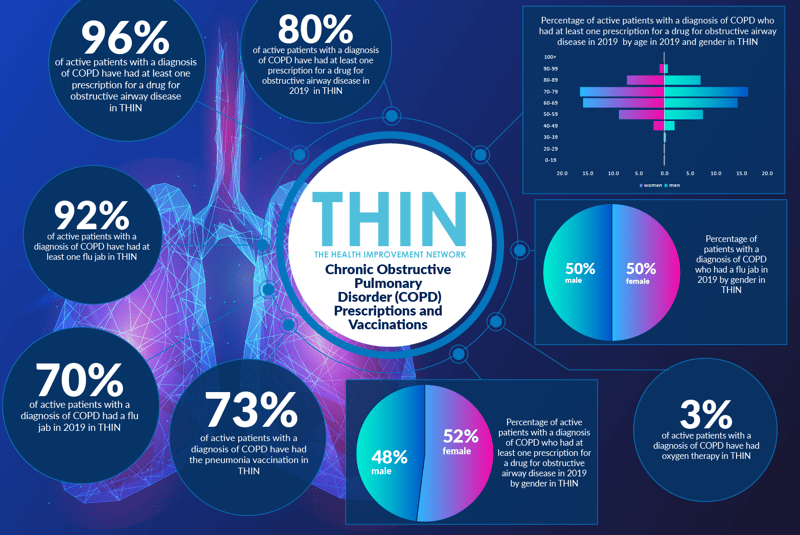
Vaccination is, of course, a high priority at the moment – and for those with COPD the annual flu vaccine is a key factor in preventing exacerbations. Analysis of THIN® data confirms that 92% of active patients with a diagnosis of COPD have had at least one flu jab; while 73% have received a pneumonia vaccination. It is important that these individuals are prioritised for the 2020 vaccines.
Asthma UK and the British Lung Foundation’s recent survey of 8,000 people with lung disease found that 35% had their respiratory care delayed or cancelled during lockdown, and around a quarter of these had respiratory symptoms worsen due to care being delayed or because they avoided using the health service.
With the peak season for COPD exacerbations approaching, THIN® data provides an invaluable resource to help clinicians to prioritise care – from overdue reviews to access to rehabilitation and, critically, any forthcoming COVID-19 vaccinations.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.