Reinforcing the value of lifestyle changes to improve liver health
Liver disease is on not just on the rise – it is the now biggest cause of death in those aged between 35 and 49, according to the British Liver Trust. Since 1970, deaths due to liver disease have increased by 400% - and over 40 people die from liver disease in the UK every day.
And yet 9 in 10 cases of liver disease can be prevented with simple lifestyle changes. Alcohol-related liver disease accounts for 60% of all liver disease; however with the rise in obesity, cases of fatty liver disease (NAFLD) are also on the increase. Experts predict that over the next decade, NAFLD will become the leading cause of end stage liver disease and liver transplantation.
During the COVID-19 pandemic, over a third of UK adults confess to having gained weight – while 44% have increased their alcohol consumption. Which is why this year’s Dry January - the annual movement through which millions of people give up alcohol for the month of January – and Love your Liver awareness are extremely pertinent.
Escalating Alcohol Reliance
Britons have drunk more alcohol and smoked more cannabis due to loneliness, depression and anxiety during the pandemic, according to a leading study of drug-using behaviour. Almost half (48%) of British respondents to the Global Drug Survey (GDS) disclosed they were drinking more alcohol than before the coronavirus outbreak. Although there are many causes of liver disease, drinking alcohol to excess is the leading cause of liver disease and liver cancer in the UK.
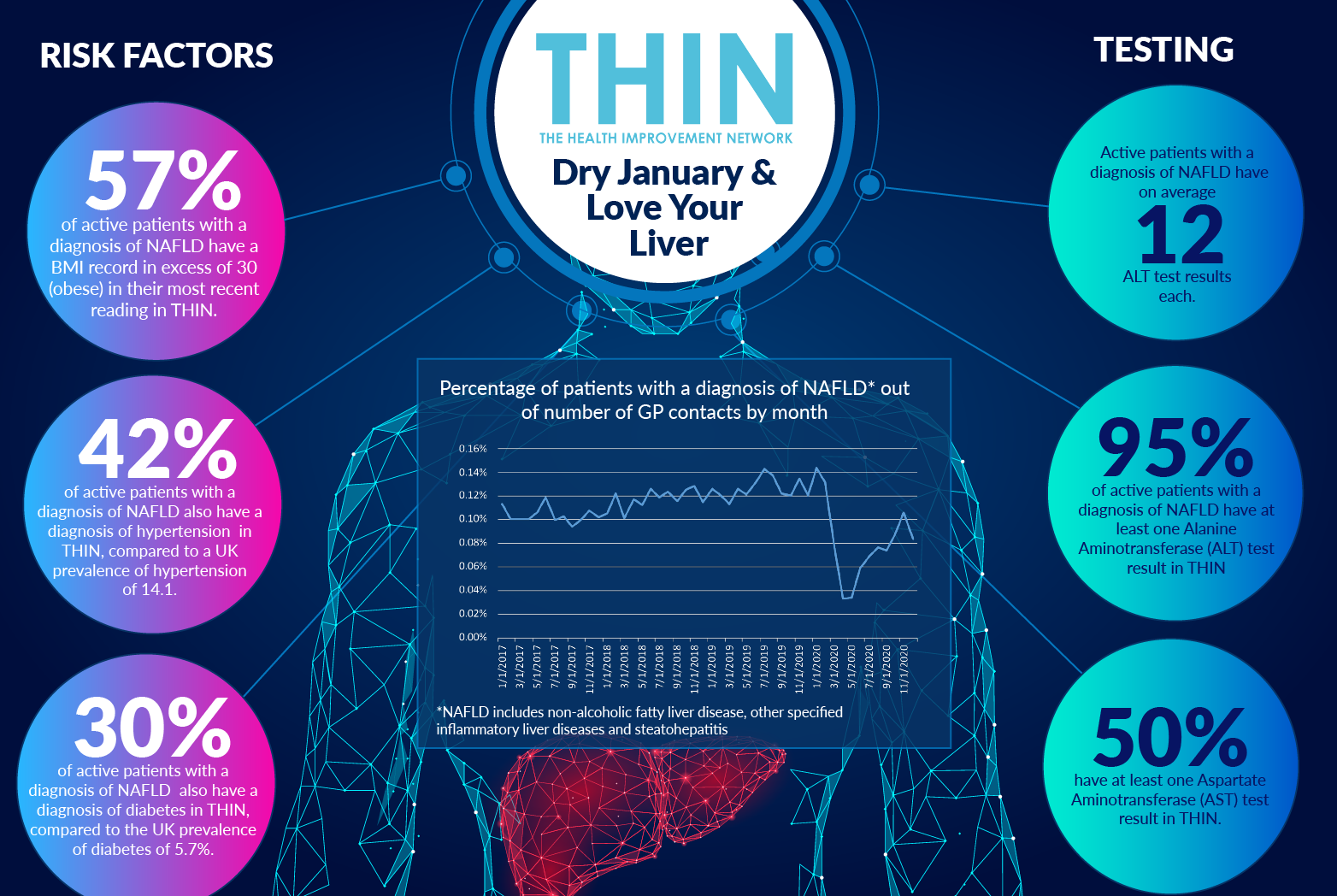
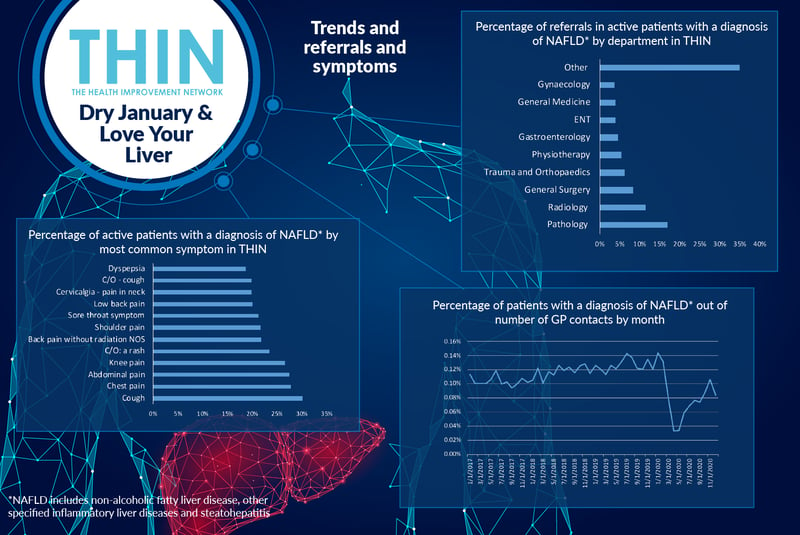
They have also eaten more - almost a third of Britons put on weight during the coronavirus lockdown. The toll on liver health is inevitable. And yet, according to analysis of The Health Improvement Network (THIN®), a Cegedim database, the percentage of GP contacts for patients with a diagnosis of NAFLD* plummeted during the first COVID-19 lockdown and had not recovered to pre pandemic levels before the next wave of lockdowns hit in November.
The concerns for those in primary care is that liver problems develop silently with no obvious symptoms in the early stages. When symptoms appear, this is most likely due to cirrhosis, or scarring, where nodules replace the smooth liver tissue and the liver becomes harder.
Identifying Liver Disease
Thousands of people are dying of liver disease unnecessarily because of late diagnosis, according to the British Liver Trust. The charity is calling for primary care liver detection and management pathways to be put in place across the UK; health checks in those aged over 40 to be routinely used to find those at risk and automated processes in GP surgeries to identify at risk patients and to manage appropriate follow-up.
Early stage symptoms include generally feeling unwell and tired all the time, loss of appetite, loss of weight and muscle wasting, feeling sick (nausea) and vomiting, tenderness/pain in the liver area, spider-like small blood capillaries on the skin above waist level (spider angiomas, blotchy red palms and disturbed sleep patterns. Red flag symptoms include fever with high temperatures and shivers, often caused by an infection, shortness of breath, vomiting blood, very dark or black tarry stools (faeces) and periods of mental confusion or drowsiness.
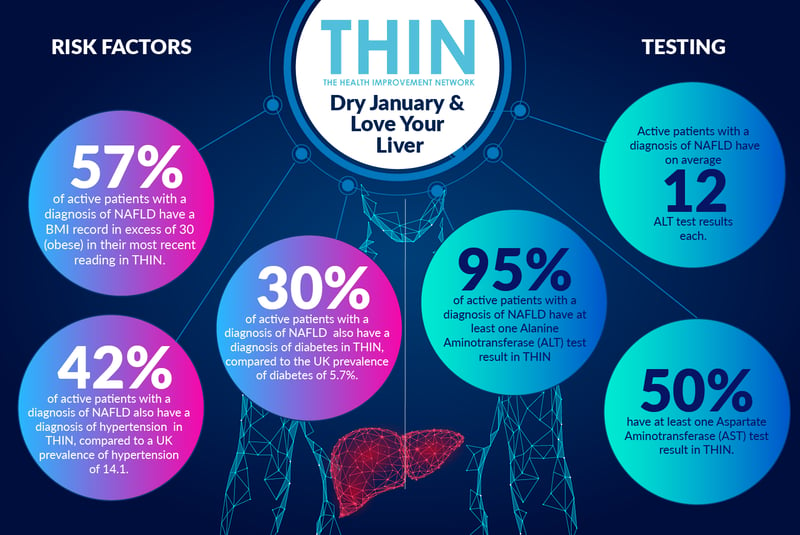
Analysis of THIN® data confirms 30% of patients with a diagnosis of NAFLD, also had a cough, 28% chest pain and 28% abdominal pain. Both hypertension and diabetes are notable comorbidities: 42% of active patients with a diagnosis of NAFLD also have a diagnosis of hypertension in THIN®, compared to a UK prevalence of hypertension of 14.1. In addition, almost one third (30%) of active patients with a diagnosis of NAFLD also have a diagnosis of diabetes in THIN®, compared to the UK prevalence of diabetes of 5.7%.
Lifestyle Change
The importance of liver health cannot be overstated. It carries out over 500 functions, from fighting infection and disease to destroying poisons and drugs, cleaning the blood, controlling cholesterol and processing food once it has been digested.
The liver also an amazingly resilient organ – given the chance. The value of reducing alcohol intake has been proven again and again. According to Alcohol Change, after just one alcohol free month 70% of people sleep better and 65% notice generally improved health. Furthermore, month alcohol-free has a lot of benefits: research published in 2018, conducted by the Royal Free Hospital and published in the British Medical Journal, found that cutting out alcohol for one month lowers blood pressure, reduces diabetes risk, lowers cholesterol and reduces levels of cancer-related proteins in the blood.
Making changes in lifestyle over just four weeks can also have wider implications of people’s attitudes to alcohol - research conducted by the University of Sussex found that six months after Dry January more than 70% are still drinking more healthily.
Furthermore, according to the British Liver Trust, there is good evidence to show that losing 10% of body weight improves liver function in those with NAFLD. Analysis of THIN® data confirms that 57% of active patients with a diagnosis of NAFLD have a BMI record in excess of 30 (obese) in their most recent reading in THIN®.
Proactive Advice
Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST) tests are key to confirming and tracking the progress of liver disease. The ALT and AST enzymes found in the liver cells (hepatocytes) which leak into the blood stream when the liver cells are damaged and indicate the degree of inflammation present in the liver.
The ALT ‘value’, or level, is more specific to the liver than the AST value because the AST value may also be high if there is muscle damage elsewhere in the body. Monitoring levels of these enzymes can help doctors assess the level of liver scarring.
Analysis of THIN® data confirms that 95% of active patients with a diagnosis of NAFLD have at least one Alanine Aminotransferase (ALT) test result in THIN® and 50% have at least one Aspartate Aminotransferase (AST) test result in THIN®. Reinforcing the importance of routine tracking and monitoring, THIN® confirms that active patients with a diagnosis of NAFLD have on average 12 ALT test results each.
The rise in alcohol use and weight gain during the pandemic will have an effect on liver health and the challenge for primary care services will be to prioritise care and rapidly identify those most at risk. This is where anonymised longitudinal data resources such as THIN® as so valuable – providing both the means to identify patients and understand the value of different lifestyle interventions in managing liver health.