Understanding Asthma and COVID-19
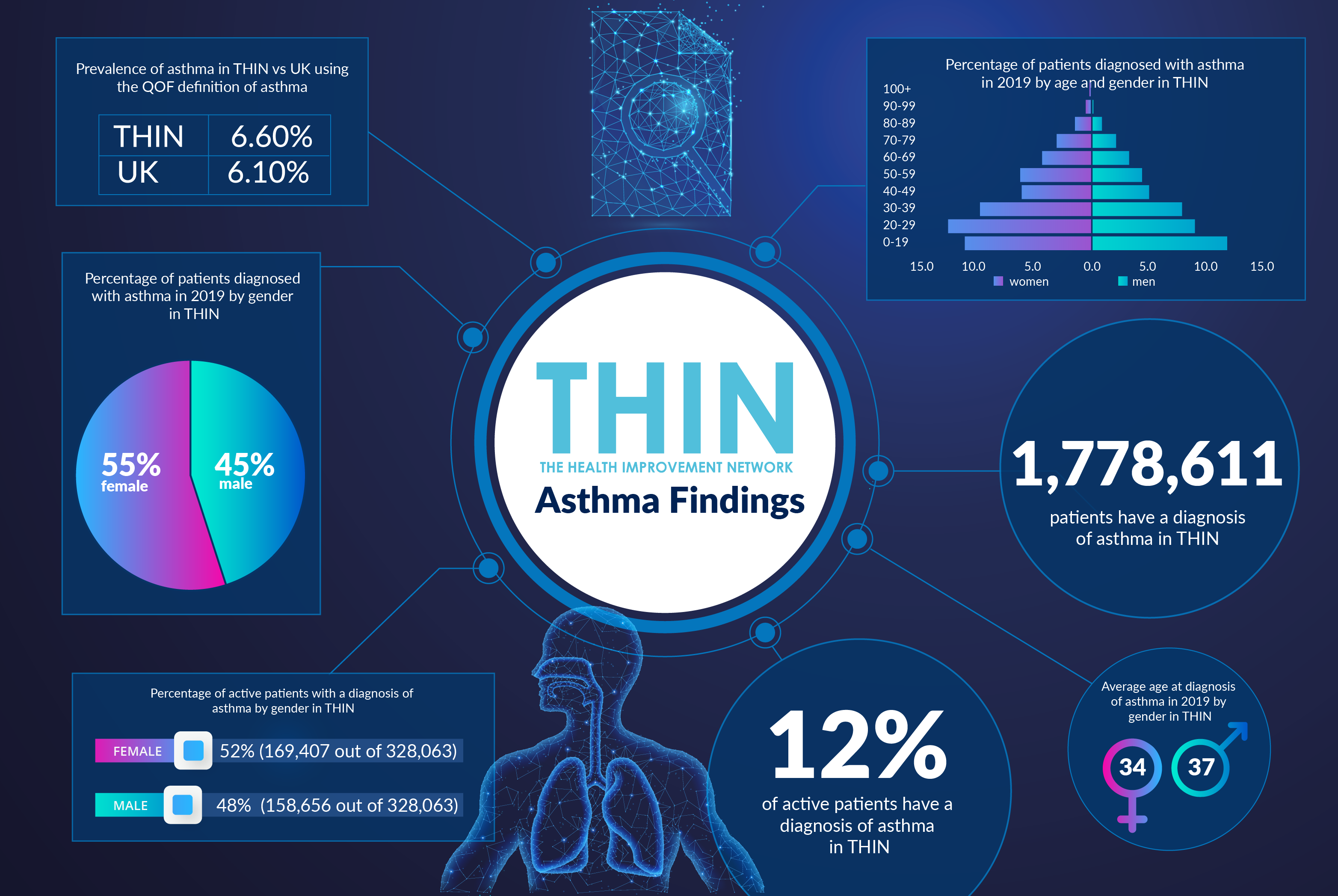
With the world’s attention now focused on a global pandemic that primarily affects the respiratory system, the 5.4 million people in the UK currently receiving treatment for asthma, including 1.1 million children, already understand the dangers of compromised airways. According to Asthma UK, three people die from an asthma attack every day – and two thirds of these deaths are preventable.
While World Asthma Day, May 5th 2020, is about raising awareness of the condition, from treatment to management, it is also hoped that new insight will be gained from the huge global research effort into understanding COVID-19, and the potential vulnerability of those with asthma, COPD and diabetes.
Fatal Condition
A chronic lung condition that affects the airways and causes inflammation which lead to spasms and narrowing of the airways, asthma sufferers endure wheezing, breathlessness and coughing. With triggers ranging from colds and viruses to pets, air quality, cigarette smoke, cold weather, mould and pollen, someone in the UK experiences a potentially life-threatening asthma attack every 10 seconds.
200,000 people in the UK suffer with severe asthma, a debilitating form of the condition that doesn’t respond to usual treatments and can cause repeated hospitalisation. Overall the NHS spends around £1 billion a year treating and caring for people with asthma.
COVID Research
Health providers globally initially raised concerns of the possible impact of COVID-19 on those with asthma, because respiratory viral infections can trigger and worsen asthma symptoms. The Asthma and Allergy Foundation of America (AAFA) warns that other strains of coronavirus can worsen asthma; while the Centers for Disease Control and Prevention (CDC) insists COVID-19 can also lead to pneumonia in people with moderate to severe asthma.
However, a new study suggests that people with asthma and allergies have reduced angiotensin-converting enzyme-2 (ACE2) gene expression and this may offer protection against severe COVID-19 illness. “Given that ACE2 serves as the receptor for SARS-CoV-2 [the virus strain that causes COVID-19], our findings suggest a potential mechanism of reduced COVID-19 severity in patients with respiratory allergies,” the study team writes in the Journal of Allergy and Clinical Immunology.
The team confirms that additional factors beyond ACE2 expression modulate the response to COVID-19 in allergic individuals, and more research into these factors is likely to provide important insights into COVID-19 disease pathogenesis. They also note that additional studies focusing on respiratory allergy, asthma and, perhaps, other allergic disorders are needed to gain a better understanding of the impact of underlying allergy on COVID-19 susceptibility and illness severity.
Improving Understanding
To gain long term understanding research needs to include the day to day experience of patients, both with and without asthma, from triggers to attacks and response to medication. This is where the Health Improvement Network (THIN®), a Cegedim Database, is so powerful. Providing direct access to anonymised longitudinal patient data, THIN® supports research into the patient pathway. By joining the dots and providing an in depth representation of community and population health, THIN® offers insight into the complexities of conditions such as asthma, including treatment response and comorbidities, providing vital insight into this chronic respiratory condition.
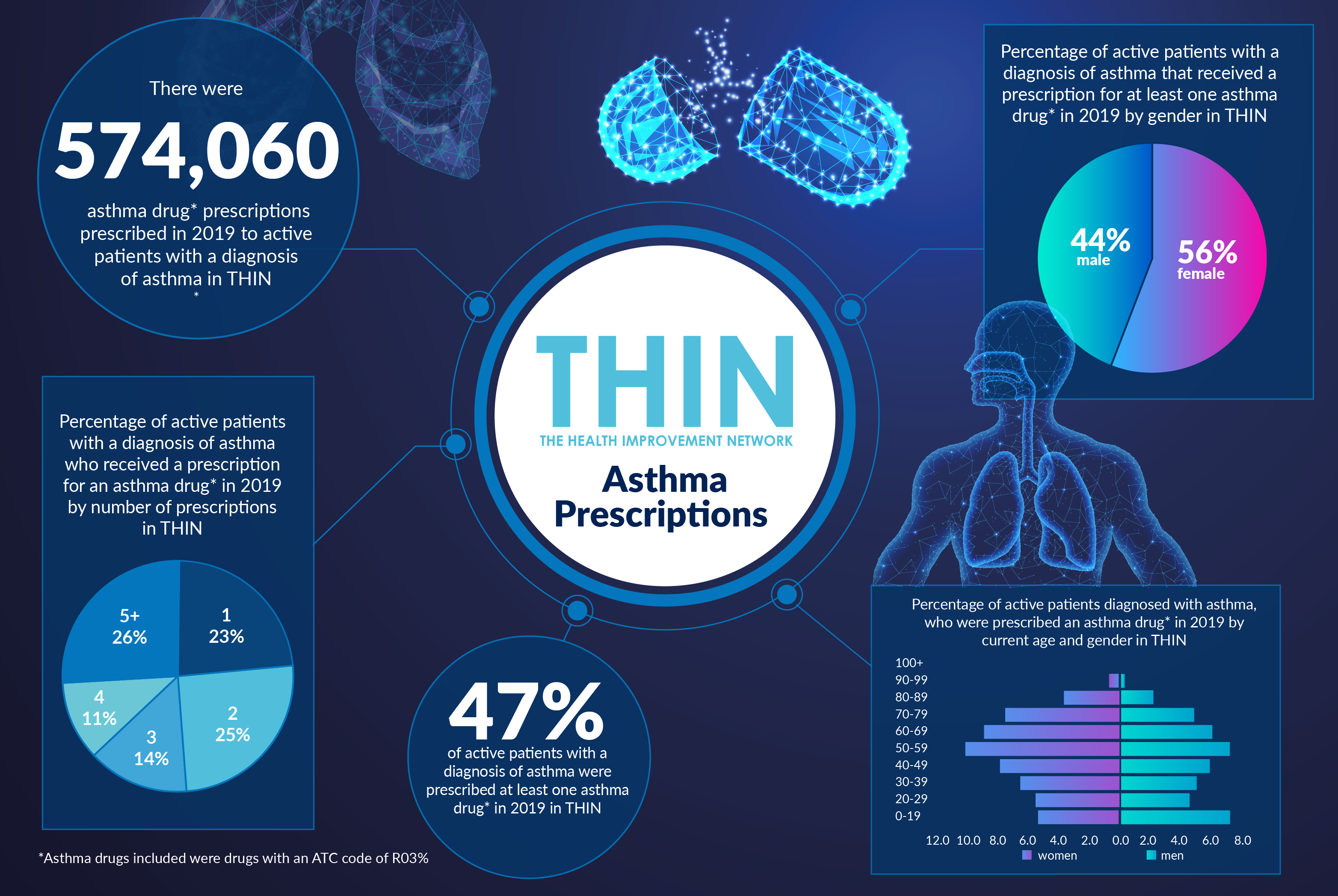
With a data history spanning almost 1.8 million patients diagnosed with asthma, analysis of the THIN® database delivers essential insight, not least into the use of drugs to manage the condition. Almost half (47%) of active patients with a diagnosis of asthma were prescribed at least one asthma drug in 2019 in THIN® – with 574,060 asthma drug prescriptions in 2019. Over a quarter (26%), received five or more prescriptions in one year.
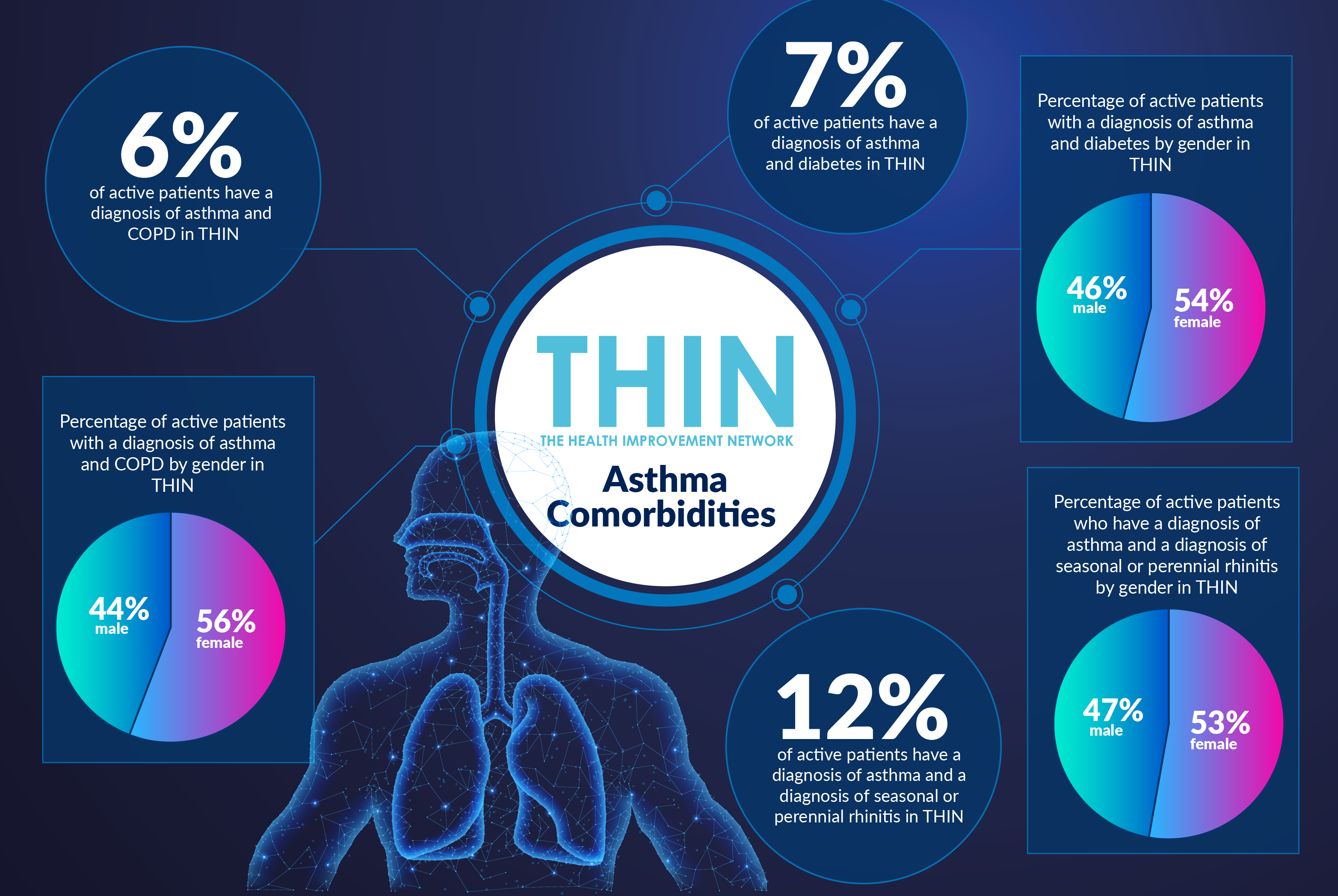
This is particularly relevant to those who also suffer from diabetes, with The Diabetes Council citing several studies that confirm people who have diabetes that is not under control or is poorly maintained are at a higher risk of developing asthma because their lung functioning seems to be weaker than those that have diabetes that is properly controlled or maintained.
These studies also concluded that people who suffer from asthma are at a higher risk of developing diabetes. The use of steroids, generally cortisone and prednisone, by asthma patients to reduce the inflammation and swelling of the airways of the lungs also affect the body’s insulin utilisation, creating additional problems for those with diabetes. In the THIN® database, 7% of active patients have a diagnosis of asthma and diabetes.
In addition, THIN® confirms that some (6%) patients suffer from both asthma and COPD. While these can be treated by the same medication, a dual diagnosis can also lead to patients being placed in multiple medications.
Even before COVID-19, the number one priority in Asthma UK’s current research strategy was to identify, understand and better classify the different forms of asthma, their progression, and effect on airway inflammation and the immune system. Better epidemiological data can improve understanding and treatment of asthma to help both individuals and clinicians better manage the condition, whilst also feeding into the vital global COVID-19 knowledge pool.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.