Recognising Risk Factors to Prevent Life Limiting Bone Fracture
World Osteoporosis Day on October 20th highlighted the importance of raising awareness of the devastating impact of fractures on millions worldwide – and the socio economic costs to both society and healthcare systems.
Wider Healthcare Implications
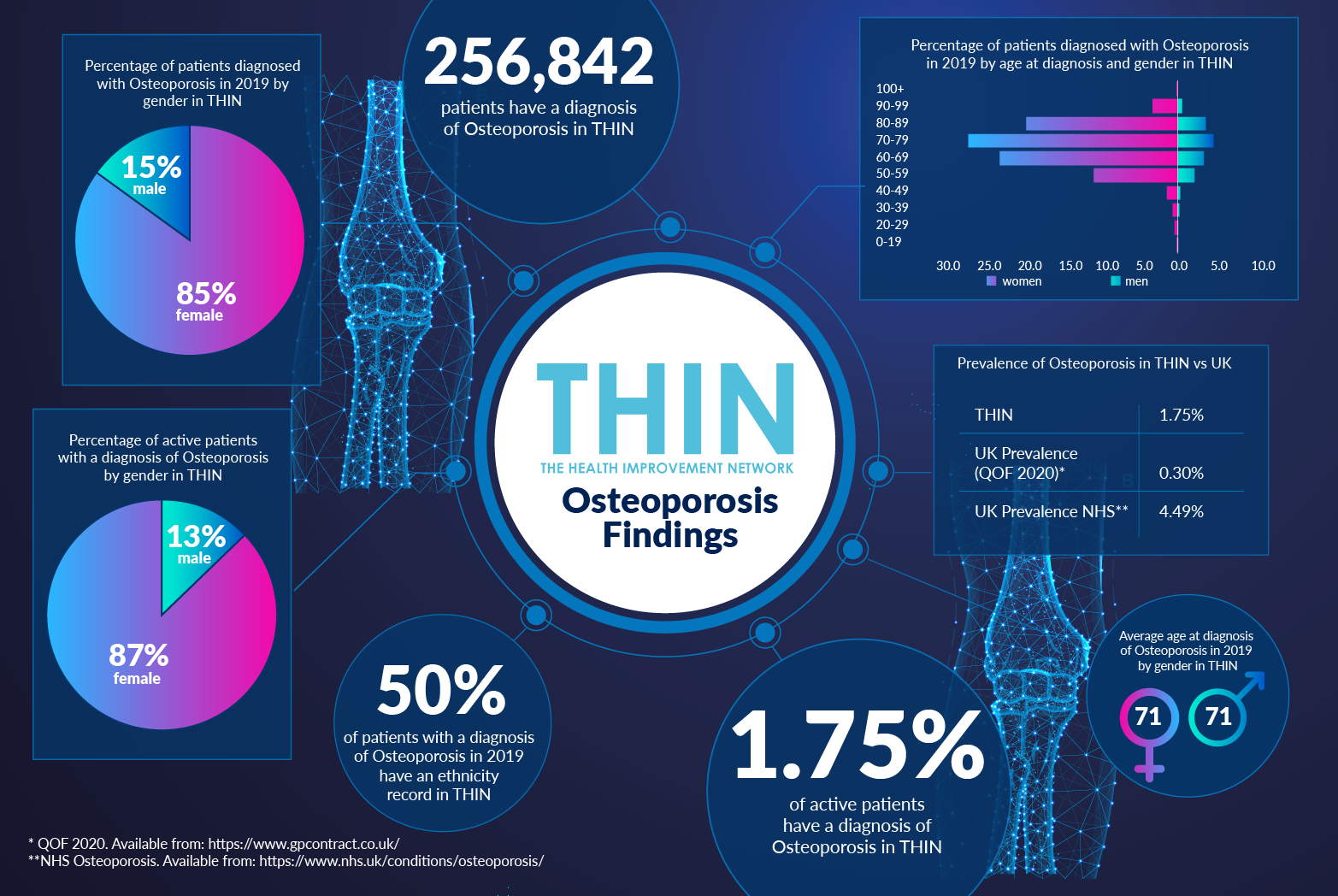
The primary risk factors associated with osteoporosis are well known: age, gender and family history. Just over a quarter of a million patients have a diagnosis of Osteoporosis in THIN® - 1.75% of active patients. The vast majority (87%) of patients with an active diagnosis of Osteoporosis are female – and the average age at diagnosis in 2019 was 71 for all patients.
According to the International Osteoporosis Foundation, despite effective medical advances to reduce fractures, a minority of men and women actually receive treatment. Only 10% of older women with fractures actually receive osteoporosis therapy. In 2010, in Europe alone some 12.3 million people were considered to be at a high risk for osteoporotic fractures were left untreated. Given the acknowledged delay in treatment as a result of Covid-19 – as well as patients being currently less willing to ‘bother’ healthcare providers, it is reasonable to suggest these figures will have increased.
Too many patients are still being diagnosed as a result of fracture – by which stage the disease has progressed, minimising the chances to reduce the life-limiting impact of osteoporosis and placing additional demands for health care providers at every level. Just consider the pain and difficulty associated with MRI or CT scan for a patient with osteoporosis - yet this can be critical in the diagnosis of other illnesses, from tumours to aneurysm. How can a patient with chronic osteoporosis be intubated without risk of breaking a bone?
While age and gender are clearly significant factors in osteoporosis, it is also important to take into account the other risk factors – including previous fracture history and hypertension.
Comorbidities Confirmed
There is growing evidence of a link between hypertension and osteoporosis – with a recent report highlighting that bone loss is associated with blood pressure in older women and that hypertension increases the incidence of hip fracture in women. These findings are confirmed by THIN® data - 43% with a diagnosis of osteoporosis in THIN® also have diagnosis of hypertension.
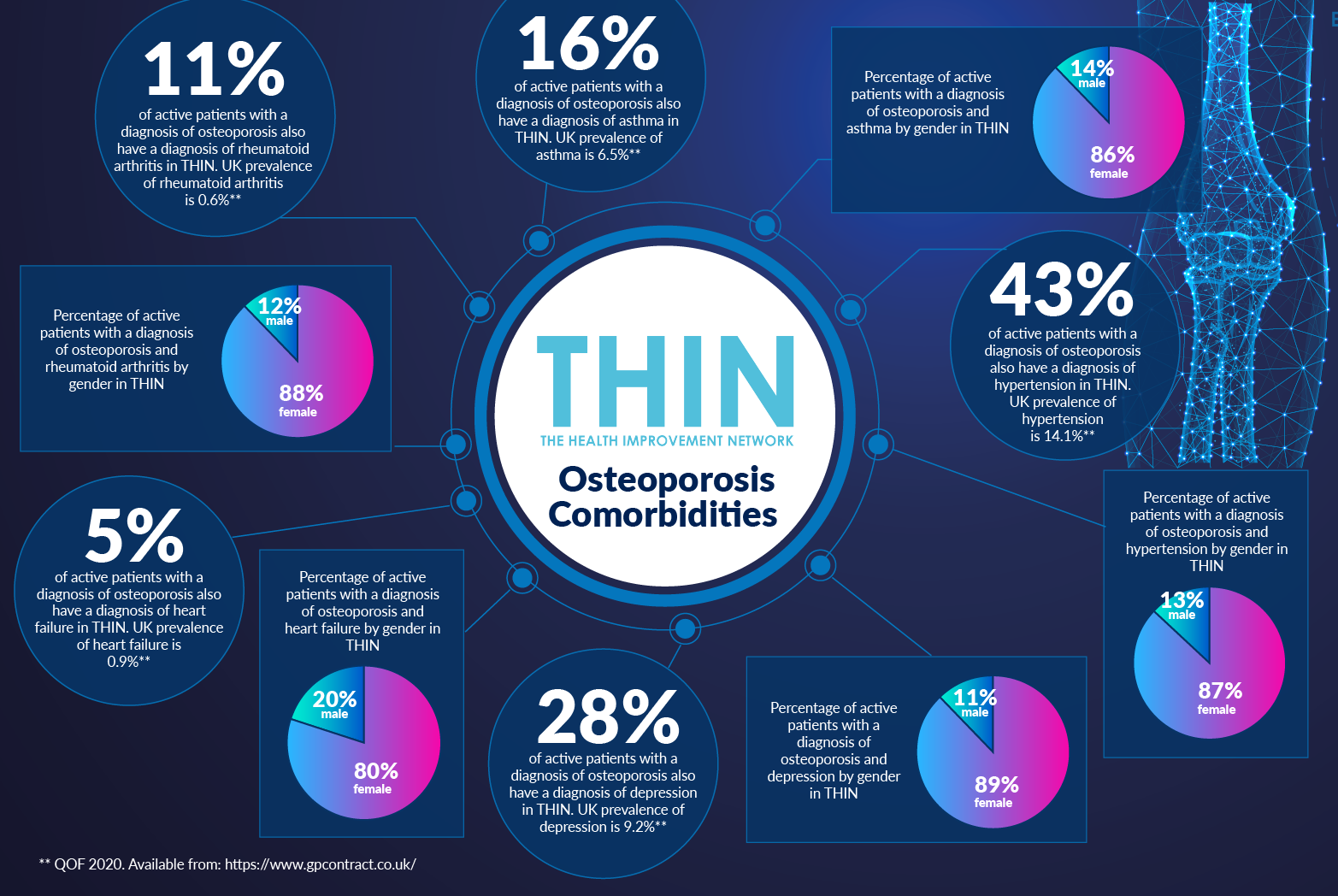
Other relevant comorbidities include asthma - 16% of patients with a diagnosis of osteoporosis in THIN® also have diagnosis of asthma. Over one in ten (11%) of active patients with a diagnosis of osteoporosis also have a diagnosis of rheumatoid arthritis in THIN®; and 5% of patients with a diagnosis of osteoporosis in THIN® also have diagnosis of heart failure.
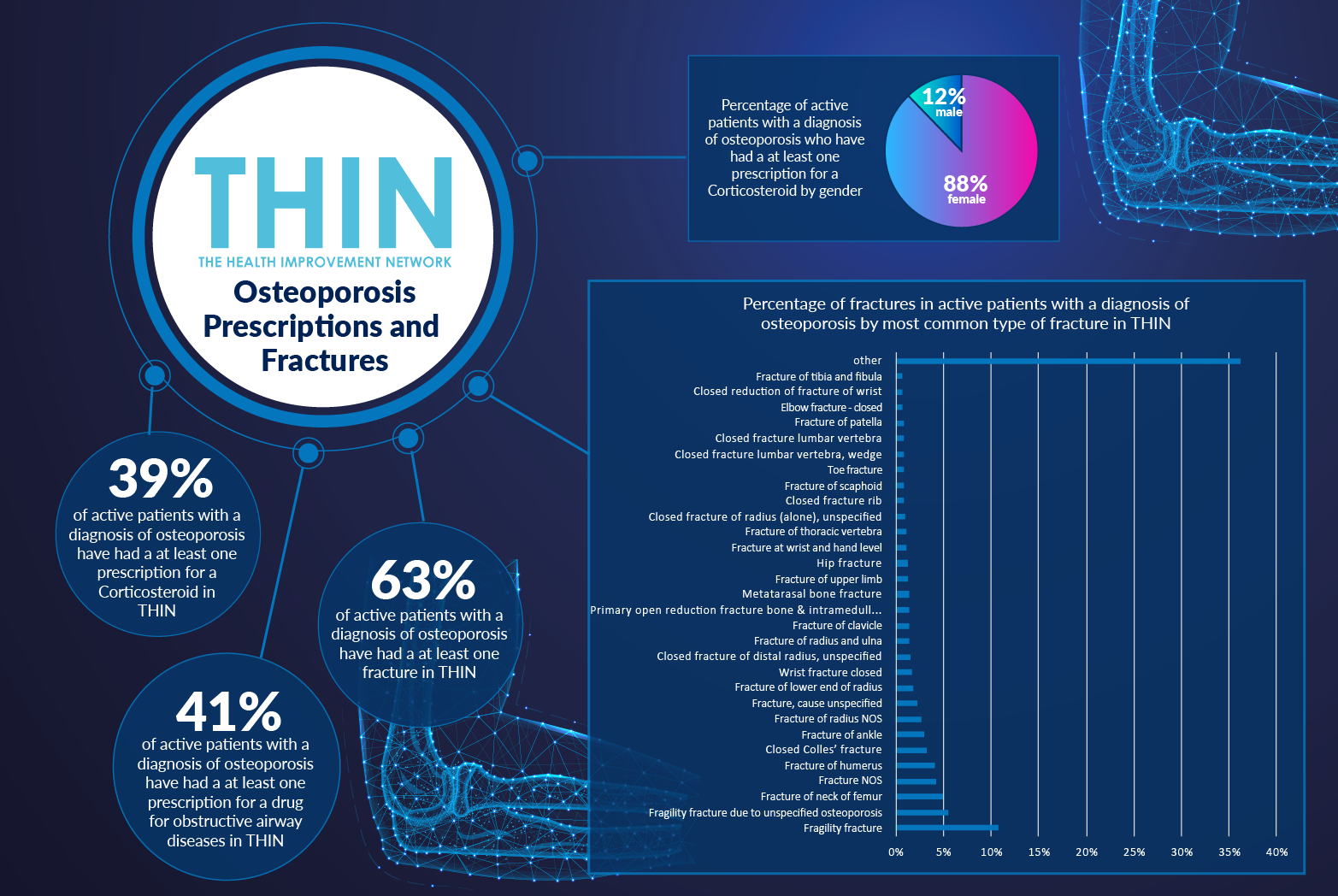
The implications of certain drugs on bone density is also confirmed by the THIN® data: 41% of active patients with a diagnosis of osteoporosis have had a at least one prescription for a drug for obstructive airway diseases in THIN®; while 39% of active patients with a diagnosis of osteoporosis have had at least one prescription for a Corticosteroid in THIN®.
The need to consider these factors to gain early – pre-fracture – diagnosis of osteoporosis was highlighted in the report which concluded: “At the minimum, patients with hypertension, and particularly older men and post-menopausal women should be screened for osteoporosis and treatment initiated when appropriate.”
Testing and Treatment
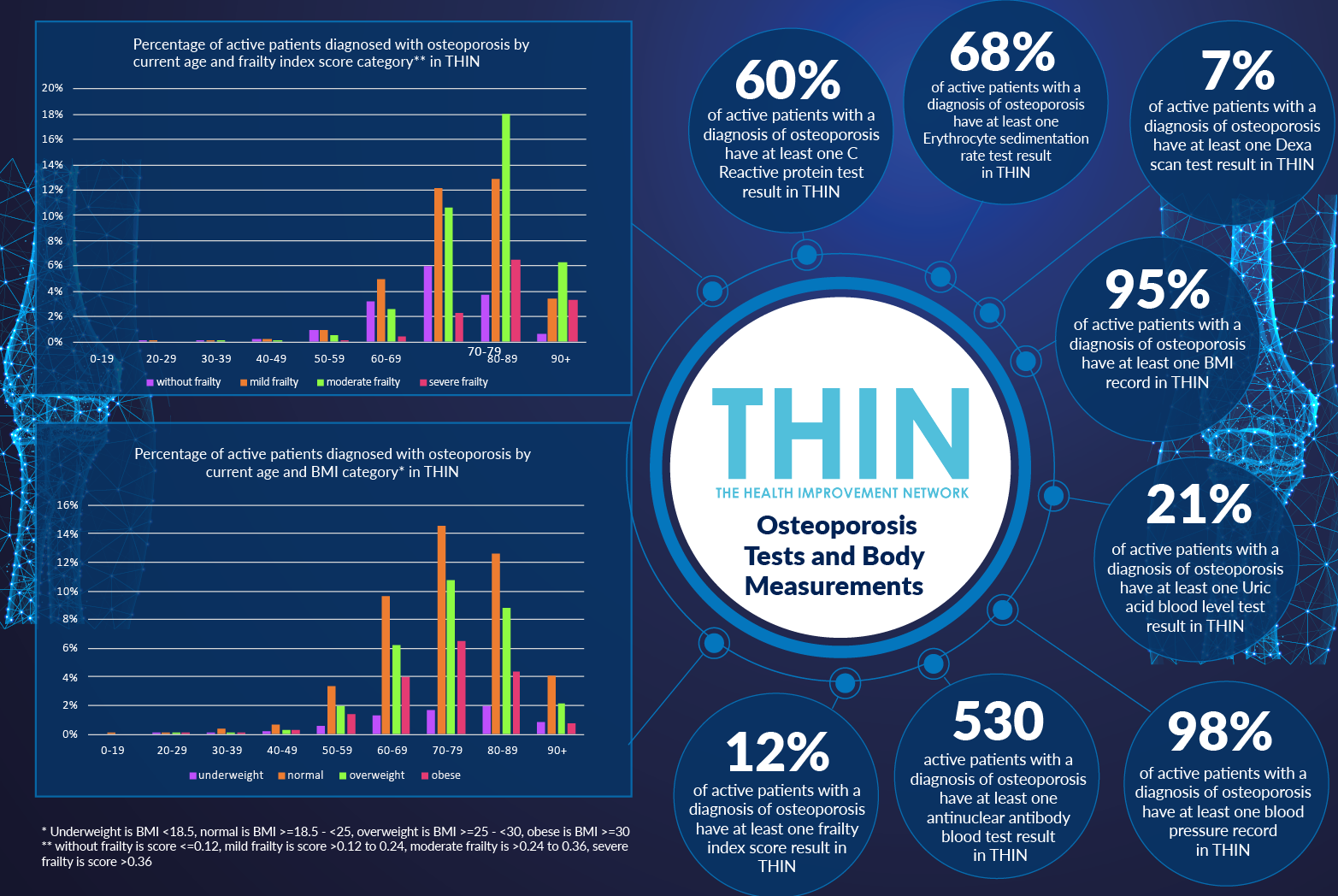
It is positive to discover that 98% of active patients with a diagnosis of osteoporosis have at least one blood pressure record in THIN®. This information can be used within population health management systems, such as Cegedim’s Outcomes Manager, to support GPs in early identification of those with a high risk of osteoporosis.
Testing for osteoporosis is well established – primarily through the use of a Dexa bone density scan. However, just 7% of active patients with a diagnosis of osteoporosis in THIN® have at least one Dexa scan; and just 12% of active patients with a diagnosis of osteoporosis have at least one frailty index score result in THIN®.
Tests for inflammation are more common, highlighting a link between inflammation and osteoporosis: 68% of active patients with a diagnosis of osteoporosis in THIN® have at least one Erthrocyte sedimentation rate test in THIN®, while 60% of active patients with a diagnosis of osteoporosis have at least one C Reactive protein test result in THIN®. In addition, 530 active patients with a diagnosis of osteoporosis have at least one antinuclear antibody test result in THIN®.
In addition to advising lifestyle changes – increasing weight bearing exercise and raising Vitamin D levels – treatments for osteoporosis are well established. The issue is diagnosis – early diagnosis. By extending the accepted osteoporosis risk factors beyond age and gender to include hypertension and asthma, as well as those diseases requiring steroid treatment, healthcare professionals have the chance to achieve early intervention – intervention that may enable individuals to avoid developing osteoporosis at all. This is not an inevitable disease – and a better understanding of the broader risk factors combined with strong population health management provides a chance to avoid millions of individuals enduring this life limiting condition.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.