Improving Lupus Diagnosis

There is no cure for Lupus (Systemic Lupus Erythematosus) but symptoms can improve if treatment starts early. The challenge for clinicians is that Lupus presents with so many very different symptoms – including fatigue, rash and kidney problems - which can vary widely from day to day in any one patient.
This year’s World Lupus Day on 10th May focuses on the need for improved patient healthcare services, research into the causes of and cure for Lupus, earlier diagnosis and treatment of Lupus, and better epidemiological data on Lupus globally.
Complex Diagnosis
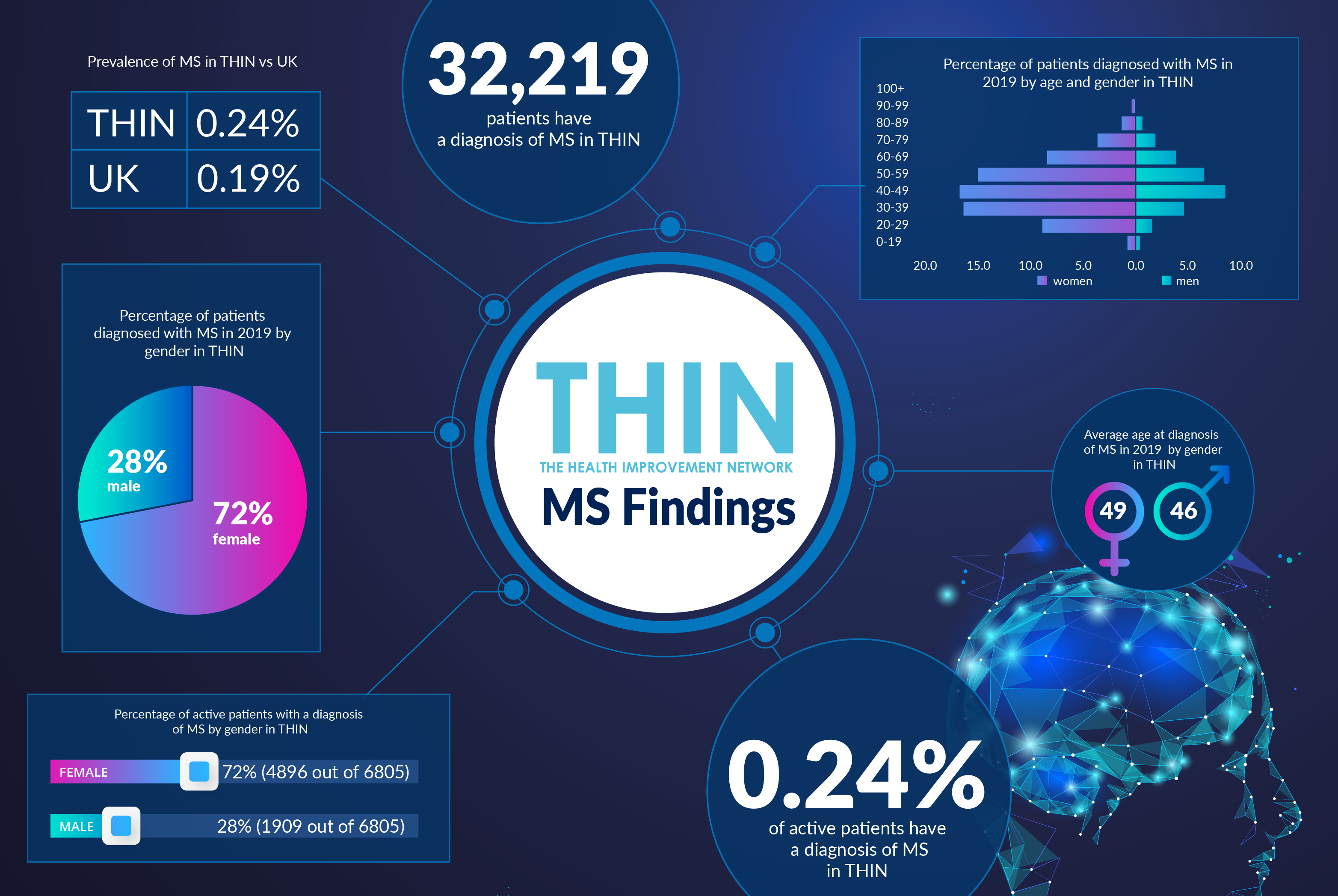
According to Lupus UK, worldwide Lupus is more prevalent than leukaemia, muscular dystrophy and muscular sclerosis (MS) – conditions which share similar symptoms - and is more prevalent in women due to hormonal change being the primary trigger for the disease. While the most common symptom is a butterfly rash on face, the auto-immune condition causes inflammation to the joints, skin and other organs.
Furthermore, not only will each patient’s profile be different but the disease can be set off by many different triggers for those susceptible. These include not only the hormonal changes at puberty, menopause and childbirth but also viral infection, sunlight and trauma, as well as a prolonged course of some medications. Furthermore there is a genetic predisposition to auto-immune conditions – with family members of Lupus patients often having conditions that include MS, thyroid problems, diabetes, Raynauds, scleroderma, Sjogrens and others.
Diagnosis is challenging, with clinicians looking for at least four of 11 internationally accepted conditions to be present either currently or at any time since the onset of the illness. The conditions are Malar rash, Discoid rash, photosensitivity, oral ulcers, Serositis, Arthritis, Renal disorders, Neurological disorders – including seizure, psychosis and balance problems, Haemotoligical disorder, immunological disorder and anti-nuclear antibody (ANA) test.
Once diagnosed, careful monitoring and a treatment programme with medication adjusted as appropriate enables the condition to be controlled, with most patients being able to live a normal life span. Only one treatment developed specifically for Lupus has received regulatory approval since the 1950’s and, depending upon an individual’s specific symptoms, typical medications range from non-steroidal, anti-inflammatory drugs (NSAIDs) to anti-malarials, steroids and immunosuppressants.
Lupus Misconceptions
To add to the difficulty for those with Lupus, the illness is poorly understood by the general public. Despite US singer and actress Selena Gomez candidly discussing her experience with Lupus, which led to a kidney transplant, more than half (51%) of the public are not aware that Lupus is a disease and almost half (48%) of those over the age of 55 have no knowledge of any complications associated with Lupus.
As a result, those with the disease can feel stigmatized, as well as isolated from family and friends, leading to additional mental health concerns. However, it is the physical limitations often created by the debilitating effect of Lupus that are a major concern: with nearly half (47%) feeling that the impact Lupus has on daily living is most misunderstood by their physician. In contrast, less than a third (30%) believed the emotional impact is most misunderstood.
Improving Life with Lupus
Almost half (47%) of those who responded to the World Lupus Federation (WLF) poll indicated they want better management and treatment options available to them through their physician. Given the complexity, variability and changeability of Lupus symptoms, better data is critical in both diagnosis and on-going management and support.
This is where the Health Improvement Network (THIN®), a Cegedim Database, is so powerful. Providing direct access to anonymised longitudinal patient data, THIN® supports research into the patient pathway. By joining the dots and providing an in depth representation of community and population health, THIN® offers insight into the complexities of conditions such as Lupus, with the variance in symptoms and day to day experience, including response to specific treatments, as well as a chance to track triggers.
While management protocols for the diverse symptoms of Lupus are established, better epidemiological data on Lupus can only support in the earlier diagnosis and treatment, which is known to improve outcomes.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.