Raising Awareness of non-motor symptoms in Parkinson's Disease
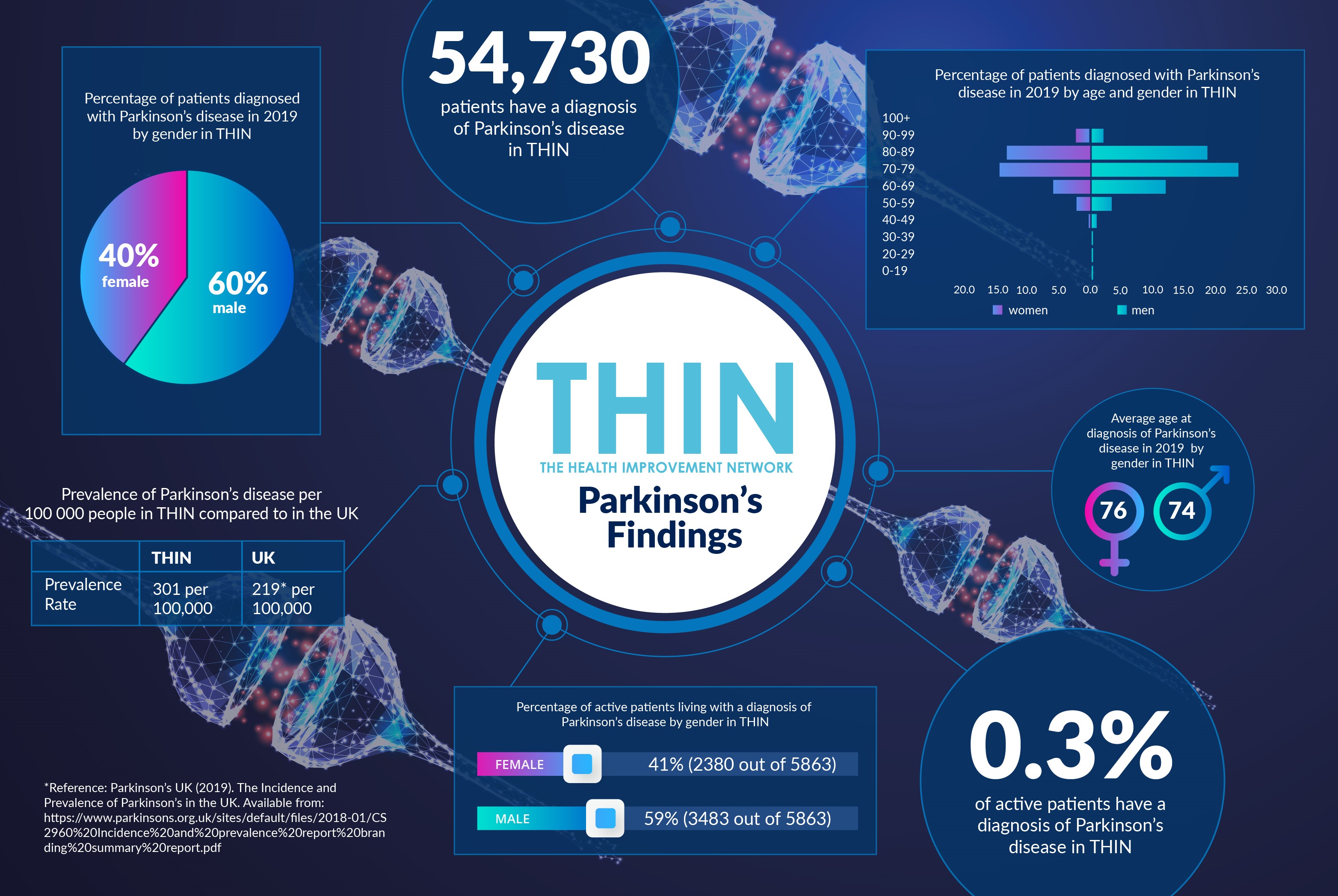
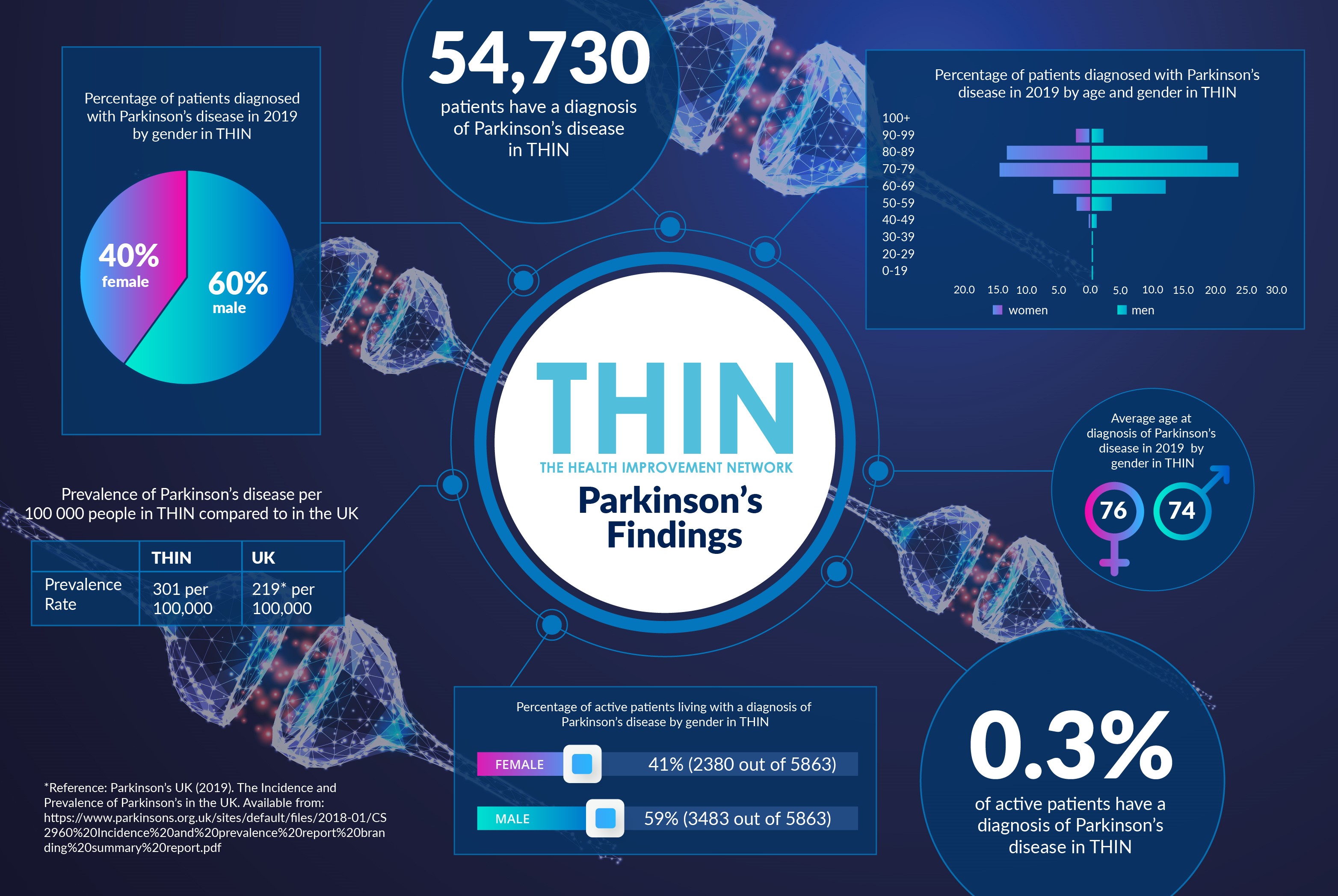
Over two hundred years since Parkinson’s disease was first described by James Parkinson in 1817, there is still no cure for this incredibly disabling illness. The progressive neurological condition affects about 145,000 people in the UK, with estimates of up to 14 million people worldwide. Not only is there no cure, but the primary treatment, the dopamine-replacement therapy Levodopa, was first developed over 50 years ago.
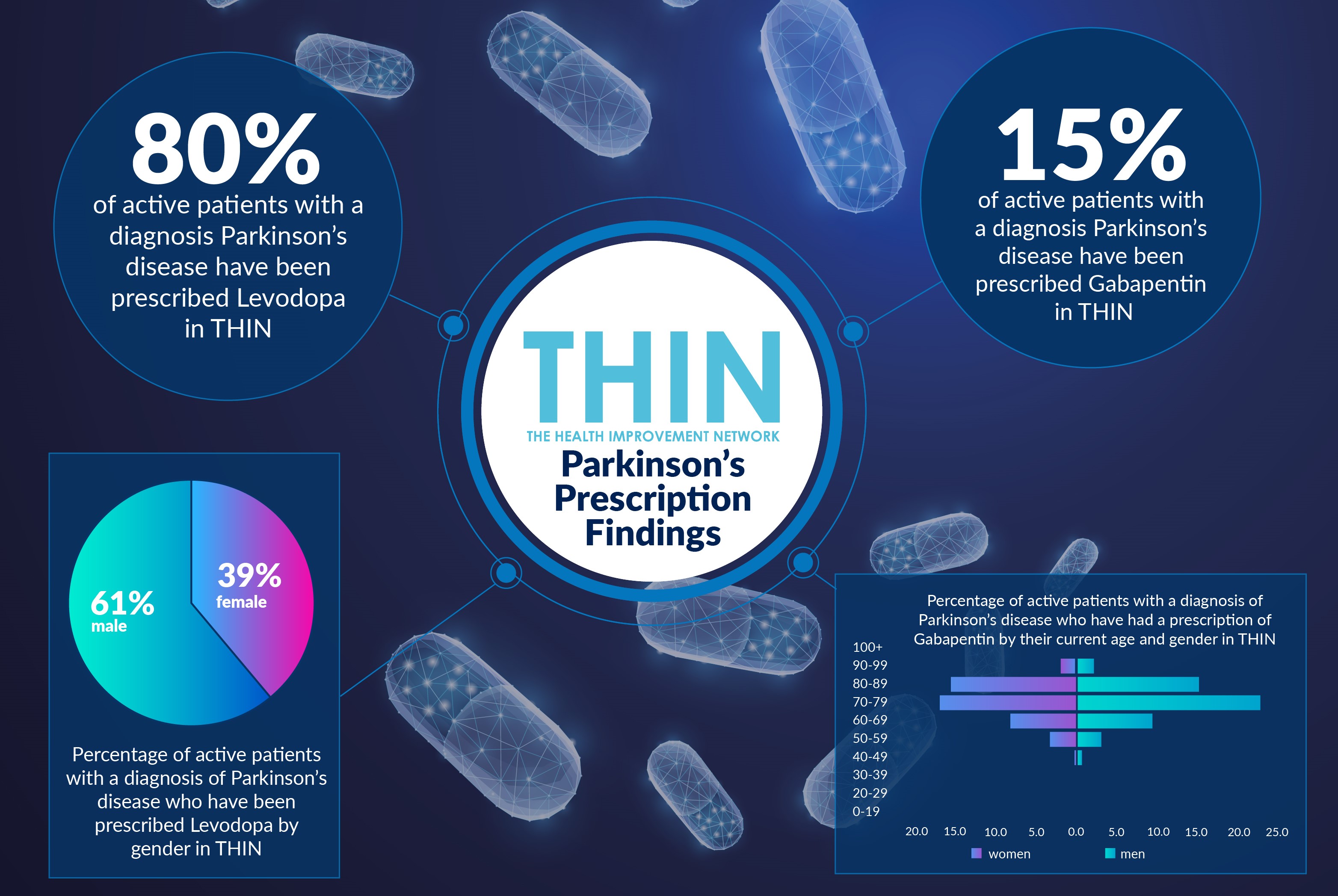
According to analysis from The Health Improvement Network (THIN®), A Cegedim Database, 80% of active patients with a diagnosis of Parkinson’s disease have been prescribed Levodopa, and 15% have been prescribed Gabapentin, a drug approved over 25 years ago to treat seizures and nerve pain. In addition, patients are encouraged to exercise and take physio-, speech and occupational therapy to help take control of the condition.
One in 66
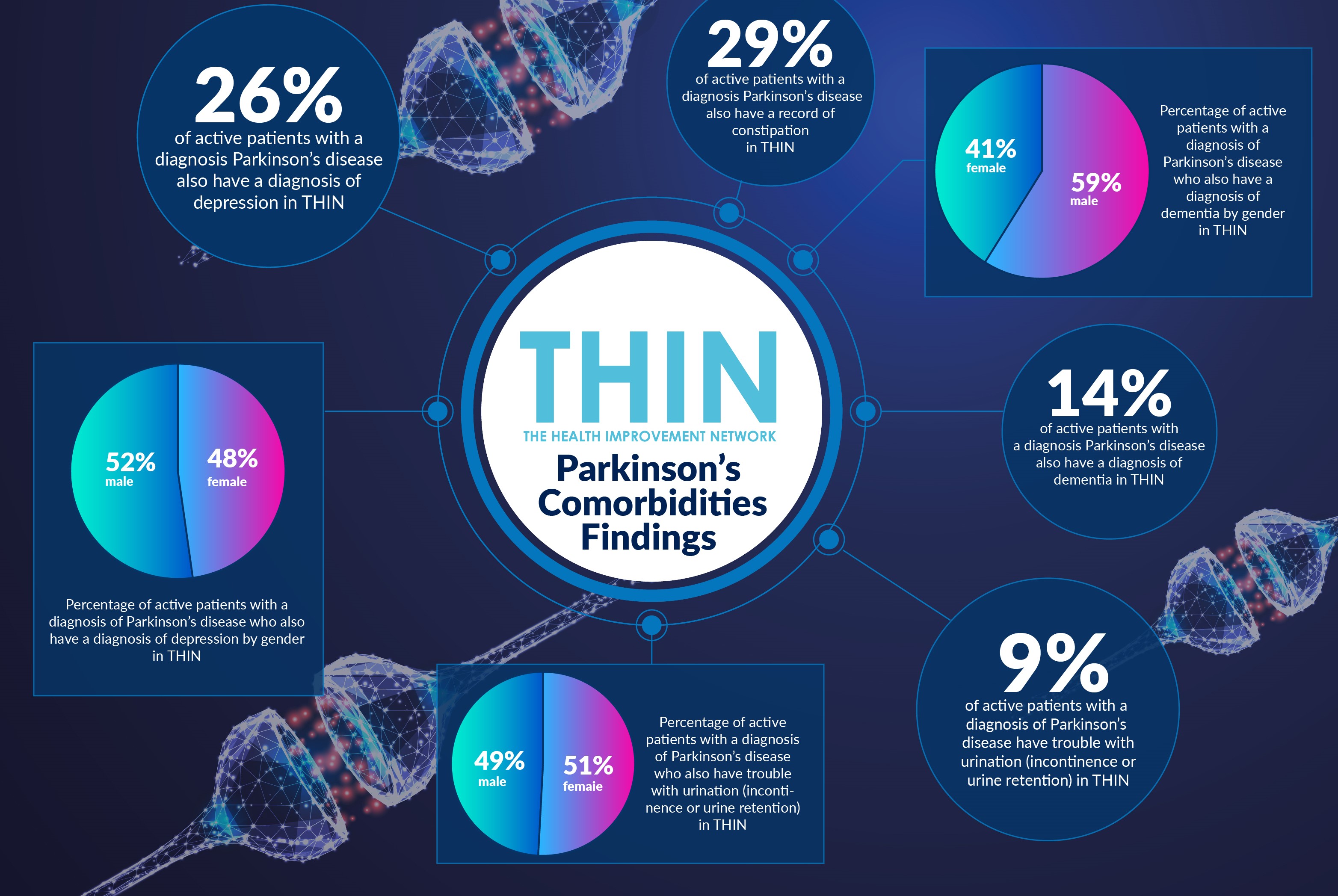
Parkinson’s affects not only those with the diagnosis. As World Parkinson’s Awareness Day highlights, more than a million people, that is one in 66, are affected by Parkinson’s in the UK – either living with it, or knowing someone who is. Men (59%) are more likely to receive a diagnosis, than women (41%) and while it is particularly prevalent in later life, with the average age for diagnosis 75, it is also seen in younger people, with 10% of cases occurring before the age of 50.
Early diagnosis is important for every illness, but with the irreversible brain damage caused by Parkinson’s and other neurological conditions, the earlier the intervention the better the chance of slowing the progress of the condition. Drugs that may slow Parkinson’s are most effective when used in the earliest stages of the condition, when there are more remaining healthy brain cells.
However, diagnosis of Parkinson’s at the early stage is difficult and there is no definitive diagnostic test at the moment. In addition there are multiple types of Parkinson’s and, while the most recognised symptoms are tremor, stiffness or slowness of movement, there is a wide range of symptoms that are associated with Parkinson’s and many do not affect movement.
Changing Focus
As Parkinson’s UK reports, there is a growing awareness of the importance of non-motor symptoms, including anxiety and trouble with memory, as well as bladder problems and constipation, all of which have a significant impact on quality of life.
According to the Centre of Excellence in Parkinson’s and Movement Disorders at King’s College, it is clear that other neuropeptides such as acetylcholine, noradrenaline and serotonin are involved right at the onset of the illness leading to a range of non-motor symptoms. Critically for early diagnosis, some of these symptoms such as hyposmia or sleep dysfunction (rapid eye movement behaviour disorder) may occur up to 10 years before the onset of motor disease.
The prevalence of non-motor symptoms is confirmed by analysis of THIN® data. Almost a third (29%) of active patients with a diagnosis of Parkinson’s disease also have a record of constipation in THIN®; while 9% have trouble with urination (incontinence or urine retention). In addition, over a quarter (26%) of active patients with a diagnosis Parkinson’s disease also have a diagnosis of depression in THIN®; while 14% also have a diagnosis of dementia.
New studies are exploring a range of relatively simple options for improving the day to day experience of those with Parkinson’s, from the use of CBD to the possible benefits of probiotics to not only improve symptoms such as constipation but also other motor symptoms of the disease.
With studies led from Kings confirming the overwhelming importance of non-motor symptoms in addressing treatment and quality of life of people with Parkinson’s, this is where THIN® can be so powerful in joining up the dots. Our data provides a clear representation of community and population health. Combining insight into non-motor symptoms such as mental health issues and constipation, can help to deliver more effective models of care for patients.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.