Movember - Changing Men's Health for 17 Years

It is time to shave off those lockdown beards and grow the now familiar ‘November Mo’. Since 2003, Movember has funded more than 1,250 men’s health projects around the world, challenging the status quo, shaking up men’s health research and transforming the way health services reach and support men. The charity raises awareness and money for men’s mental health and suicide prevention, prostate cancer and testicular cancer, with the aim of reducing the number of men dying prematurely by 25% before 2030.
This year, with Covid-19 not only resulting in delays to diagnosis and treatment but also affecting research projects and funding activity, there is a strong focus on prostate cancer – the most common cancer in men, with more than 1.3 million men diagnosed each year.
Prostate Cancer
More than 11,700 UK men die from prostate cancer each year. This year, however, risk of Covid-19 meant many men have not had conversations with their GP about their prostate cancer risk, according to Prostate Cancer UK. With referrals for prostate cancer plummeting, the charity is concerned that many men will have their prostate cancer diagnosed too late. This Movember is a chance to both improve awareness and raise funds to support those men living with prostate cancer.
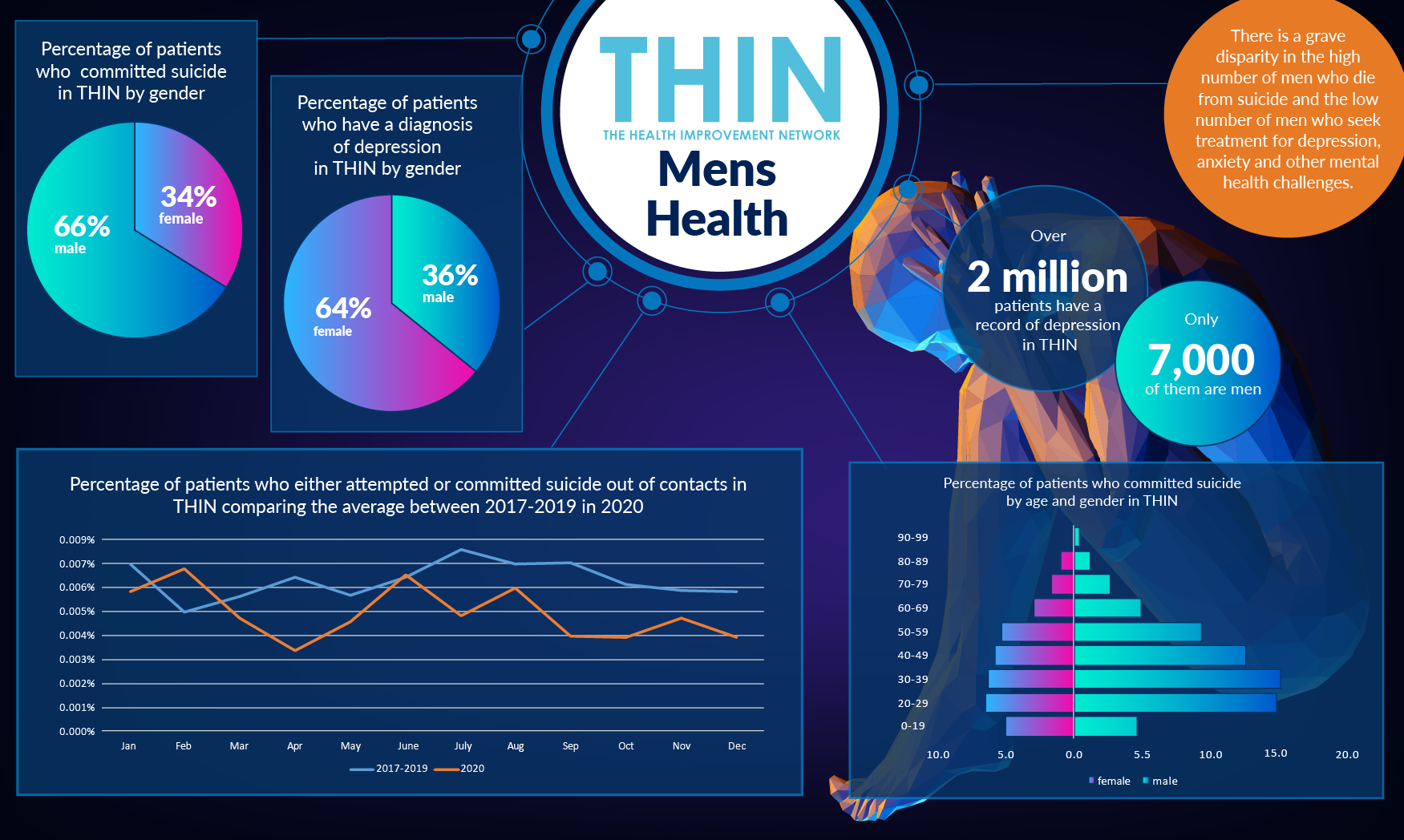
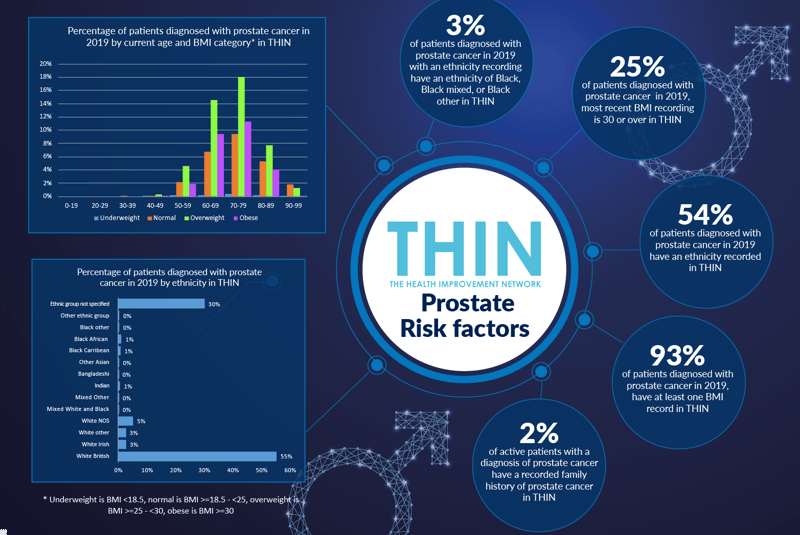
Raising awareness is one way in which comprehensive population health data, such as The Health Improvement Network (THIN®), a Cegedim database, can play a vital role by highlighting individuals who share relevant risk factors, helping healthcare professionals identify and prioritise care. Prostate cancer mainly affects the over 50’s and the risk increases with age; it also affects those with a family history of prostate cancer. However, while 1 in 8 men in the UK will get prostate cancer in their lifetime, the risk is far higher for black men – around 1 in 4 according to Prostate Cancer UK, which is funding additional research to gain further understanding into why this is the case.
Analysis of THIN® data also suggests that obesity is a risk factor. 93% of patients diagnosed with prostate cancer in 2019 have at least one BMI record in THIN® and the most recent BMI reading for 25% of patients diagnosed with prostate cancer in 2019 is 30 or over (obese). The link between diabetes and prostate cancer – along with other cancers – has also been long explored. THIN® data confirms that 17% of active patients with prostate cancer also have a diagnosis of diabetes. The typical prevalence for diabetes in men is 6%.
Living with Cancer
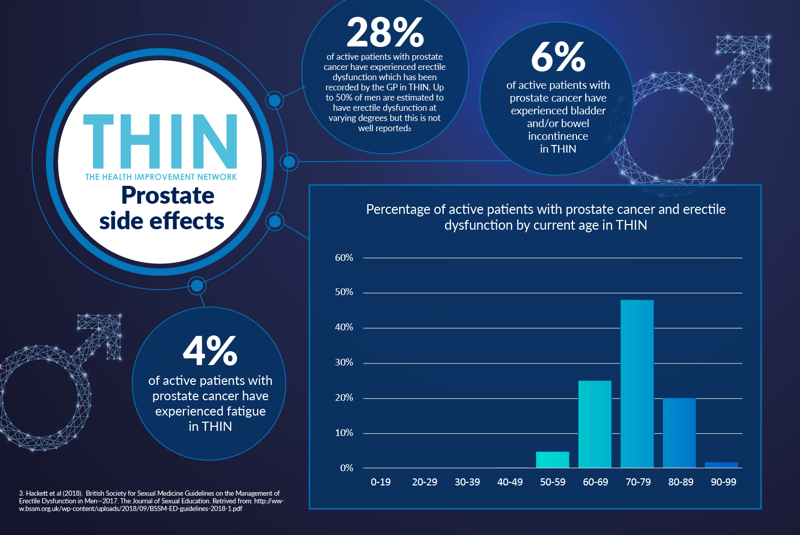
Population health data such as THIN® also plays a vital role in understanding the experience of those living with cancer. The diagnosis methods and treatments for prostate cancer are widely accepted to cause serious side effects, including erectile dysfunction and incontinence, which can deter men from seeking help when experiencing symptoms – such as trouble urinating or blood in semen.
Analysis of THIN® data confirms the challenges associated with living with prostate cancer: 28% of active patients with prostate cancer have experienced erectile dysfunction which has been recorded by the GP in THIN®. In addition, 6% of active patients with prostate cancer have experienced bladder and/or bowel incontinence in THIN®; while 4% of active patients with prostate cancer have experienced fatigue in THIN®.
As with all cancers, early diagnosis is key to improving outcomes. However, one of the problems in diagnosing prostate cancer is that symptoms are rarely experienced until the tumour has grown large enough to put pressure on the urethra. There is currently no routine screening test for men in the UK – the standard prostate-specific antigen (PSA) testing remains controversial as it can lead to men being biopsied and treated unnecessarily, either because they don’t have cancer or have a type of cancer that would not cause harm.
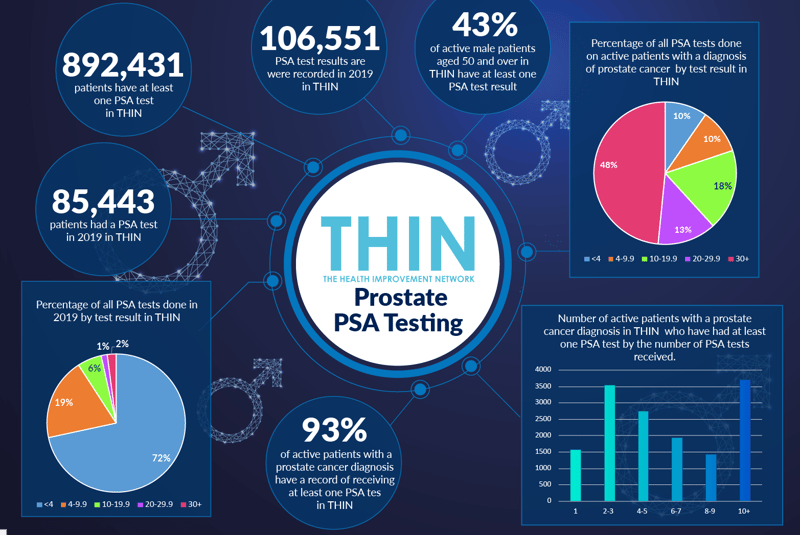
Analysis of THIN® data reveals that 43% of active male patients aged 50 and over have at least one prostate-specific antigen (PSA) test. 93% of active patients with a prostate cancer diagnosis have a record of receiving at least one PSA test in THIN®.
Changing Diagnosis and Treatment
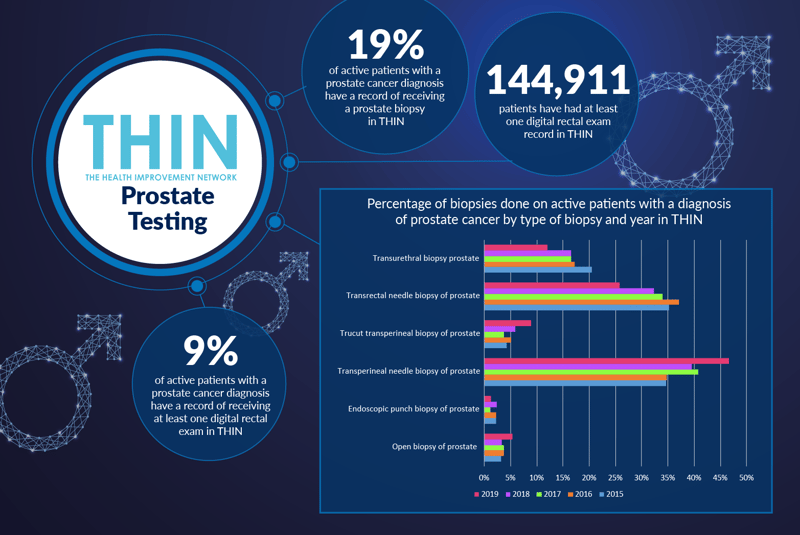
Biopsy techniques deployed to diagnose prostate cancer can result in serious side effects. THIN® data confirms that 19% of active patients with a prostate cancer diagnosis have a record of receiving a prostate biopsy in THIN®. Two types of prostate biopsy are currently used – transrectal ultrasound guided (TRUS) which accesses the prostate through the rectal wall, and transperineal (TP) biopsy which goes through the skin of the perineum. Both can now be performed under local anaesthetic- in the past TPs required general anaesthetic.
According to Prostate Cancer UK, TP biopsies have much lower rates of side effects than TRUS biopsy, especially incidence of sepsis. Analysis of THIN® data confirms the transition from TRUS to TP, with TP comprising the majority of biopsies performed in 2019.
For many men with prostate cancer, no treatment will be necessary. Where it is necessary, the aim is to cure or control the disease to minimise the impact on day to day life. Analysis of THIN® data confirms that 11% of active patients diagnosed with prostate cancer have had radiotherapy; 28% have had a prostatectomy; and 9% have had a prescription for a chemotherapy drug recorded in their primary care electronic health record in THIN®.
Conclusion
The numbers are rising – and by 2030, prostate cancer will be the most common of all cancers. Prostate Cancer UK has a four strand strategy to address this rise: improve the speed of diagnosis; improve the accuracy of diagnosis to enable better, more personalised treatment; improve available treatments and deliver better support. Population health data such as THIN® can play a vital role at every stage of this process. From highlighting the risk factors to inform diagnosis to providing better understanding of the day to day experience for men living with prostate cancer, better data is the foundation of meeting the Movember goal, namely improving men’s health.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.