Finding the missing millions with hepatitis
Hepatitis is one of the leading causes of death globally, killing more people each year than AIDS and malaria combined. While these deaths are preventable with the availability of vaccines, effective treatments and a cure for hepatitis C, only 10% of people who live with the disease are aware of their diagnosis. As a result, they may unknowingly transmit the infection to others, before possibly developing fatal liver disease.
In 2016, every government in the world made a commitment to eliminate viral hepatitis by 2030. Yet today, the World Hepatitis Alliance estimates that worldwide 290 million people are unknowingly living with viral hepatitis, which is why the theme of this year’s World Hepatitis Day on 28th July, is “Find the missing millions”.
Undiagnosed and Untreated
Most commonly caused by a viral infection, hepatitis (A-E) is an inflammation of the liver that kills 1.4 million people every year. Chronic hepatitis B and hepatitis C are life-threatening infectious diseases that may cause serious liver damage, liver cancer and premature death. It is estimated that 257 million people live with hepatitis B and 71 million with hepatitis C globally; hepatitis B and C are responsible for more than one half of all new liver cancer cases and one in every 12 cancer deaths.
Despite the global pledge to eliminate viral hepatitis, the number of deaths due to viral hepatitis is on the increase – with 1.75 million new hepatitis C infections annually. Yet the control of hepatitis B and elimination of hepatitis C are both feasible and achievable through a combination of prevention, testing and treatment initiatives. It is estimated that eliminating hepatitis B and hepatitis C by 2030 would prevent approximately 36 million infections and save 10 million lives.
Vaccination is a key part of the global strategy for eradicating hepatitis. In the UK, the hepatitis B vaccine is given to infants as part of the routine childhood vaccination schedule and those at high risk of developing the infection.
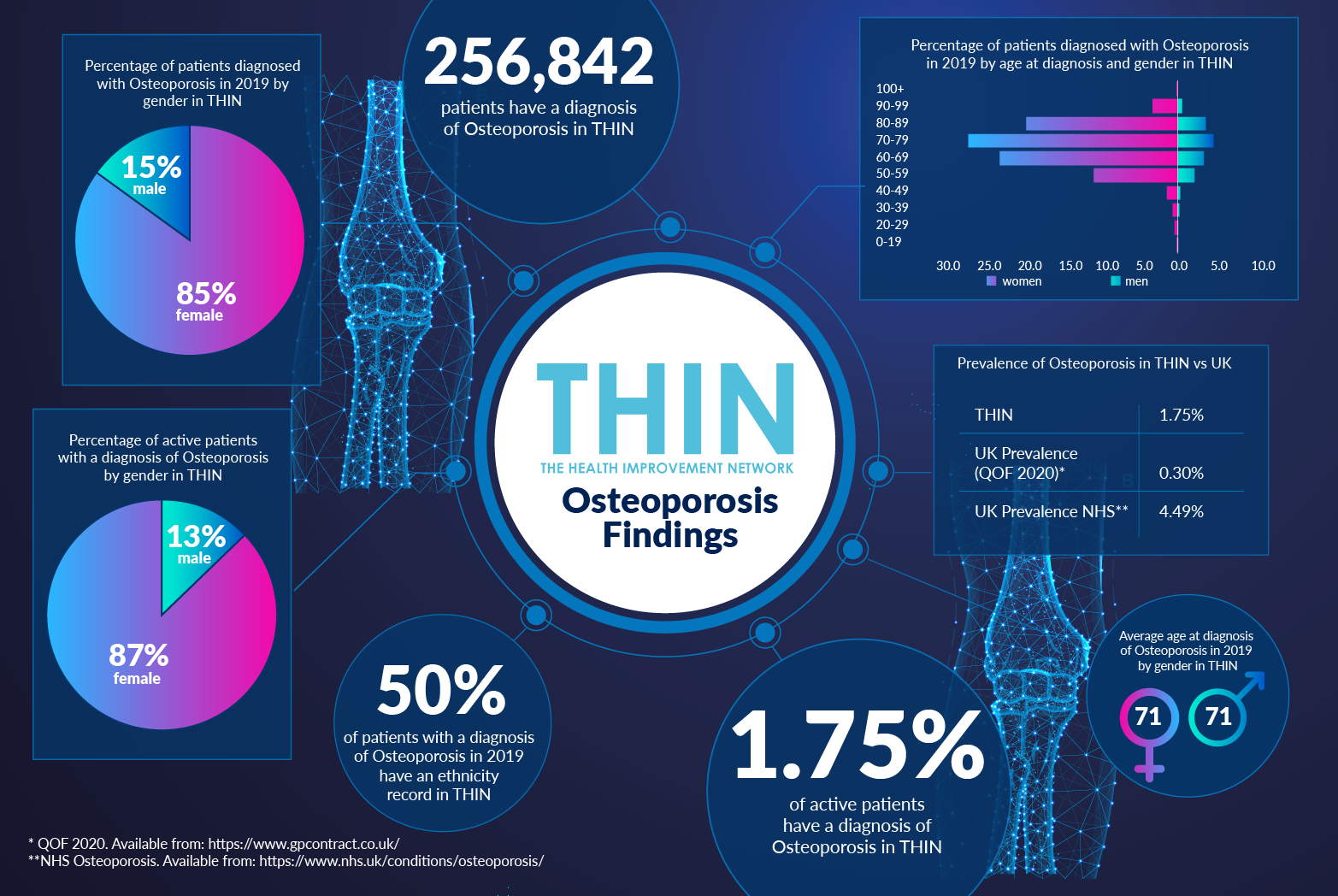
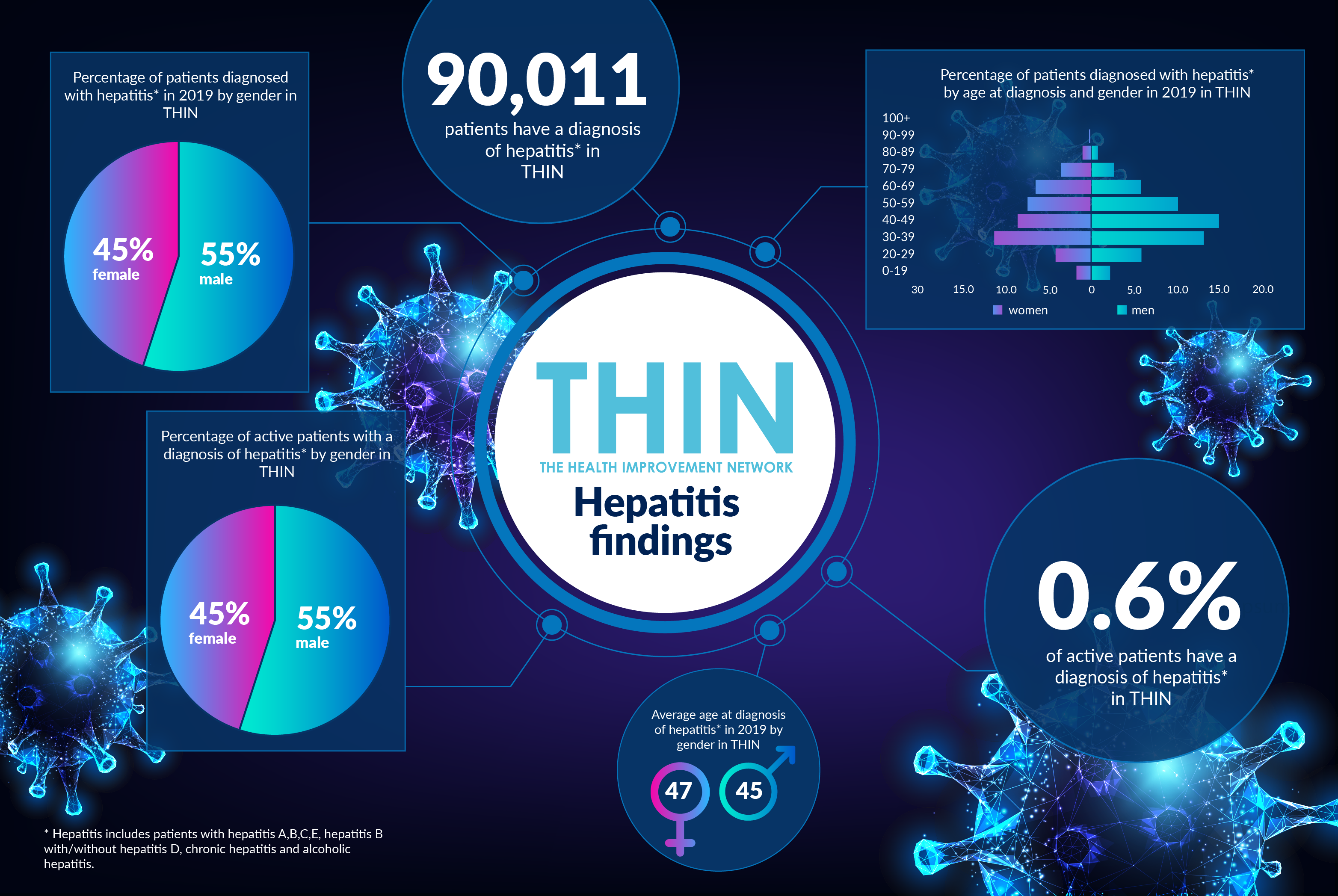
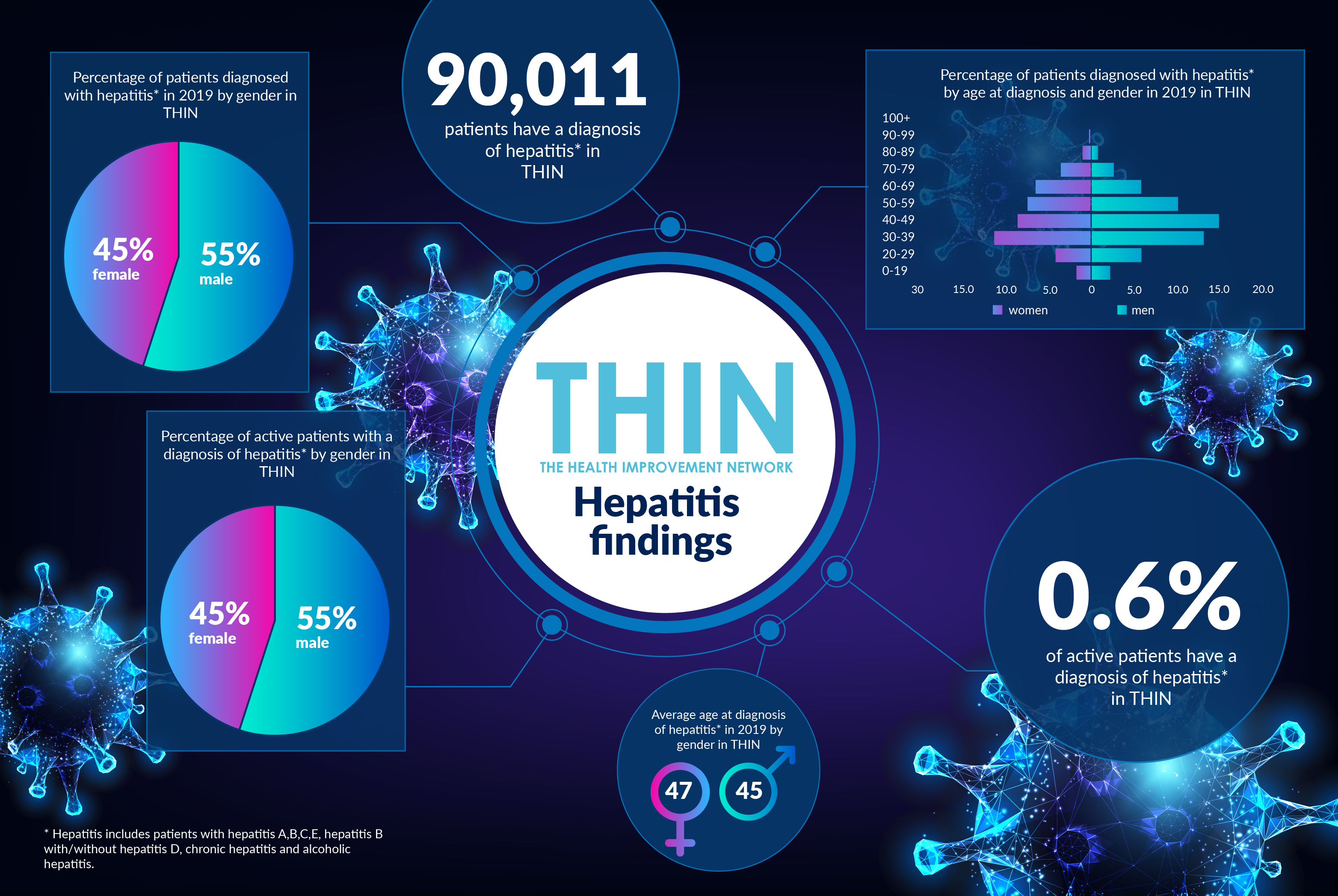
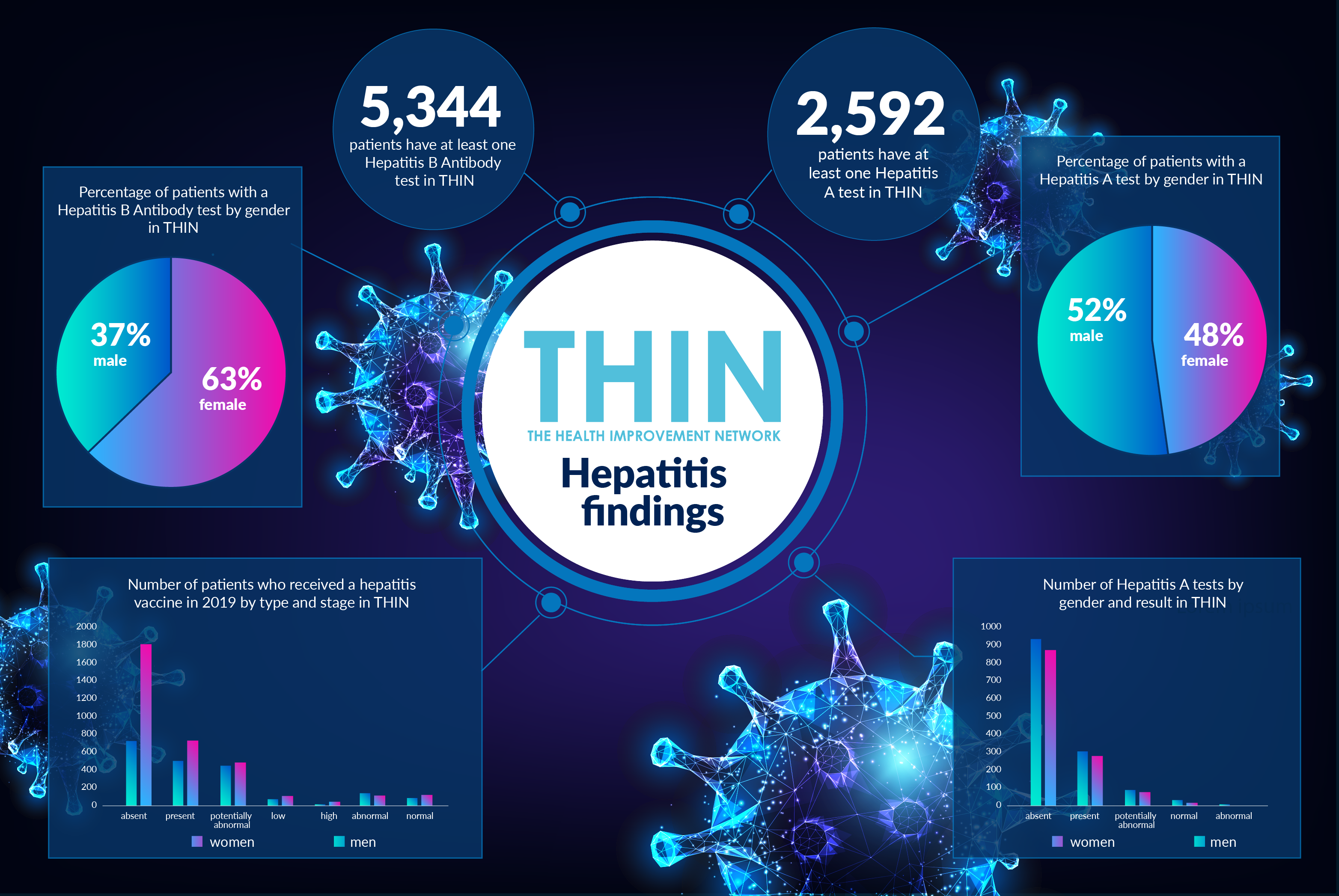
According to analysis of The Health Improvement Network (THIN®), A Cegedim Database, 90,011 patients have a diagnosis of hepatitis* in THIN®. 55% of these are male, 45% female, with the average age of diagnosis 45 for men and 47 for women. When it comes to vaccinations, however, the gender split is reversed: while 8,338 patients had at least one hepatitis vaccination in 2019, 55% were female.
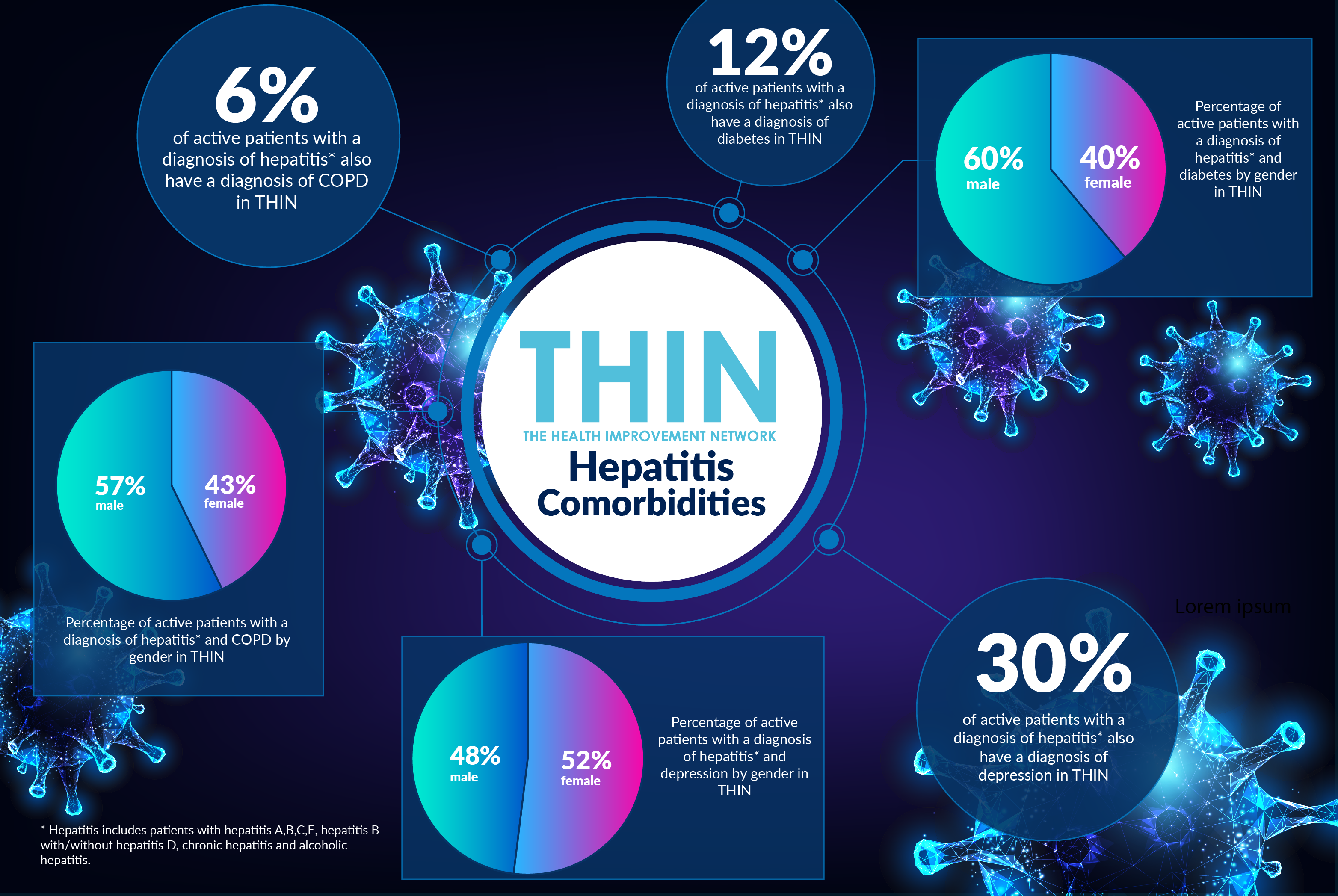
Understanding Comorbidity
Hepatitis can also affect other aspects of health. For example, the chronic form of the hepatitis C virus (HCV) has been shown to be a risk factor for the development of both type 1 and type 2 diabetes. Analysis of THIN® data reveals 12% of active patients with a diagnosis of hepatitis also have a diagnosis of diabetes in THIN. There is also growing awareness of the incidence of both Chronic Obstructive Pulmonary Disease (COPD) and hepatitis, with Brazilian researchers investigating the prevalence of Hepatitis C in patients with COPD, discovering the prevalence of Hepatitis C infection in COPD patients was 7.5%, compared to 0.41% prevalence of Hepatitis C infection in blood donors.
In addition to demonstrating a significantly greater likelihood of Hepatitis C infection in those with COPD than the general blood donation population, this research also revealed that patients with COPD had more severe lung disease when they also were infected with Hepatitis C. These findings are confirmed by data from the THIN® database: with 6% of active patients with a diagnosis of hepatitis also have a diagnosis of COPD in THIN®.
It is also important for clinicians to recognise the risk of depression associated with a hepatitis diagnosis, particularly with Hepatitis B, which is transmitted through contact with the blood or other body fluids, such as saliva, semen and vaginal fluid, of an infected person. The Hepatitis B Positive Trust confirms it receives significant contact from people fearing ongoing transmission of the virus. Analysis of THIN® data confirms the high incidence of depression: 30% of active patients with a diagnosis of hepatitis also have a diagnosis of depression in THIN.
Diagnosis and Testing
Increased diagnosis of hepatitis is one of the key actions demanded by the World Hepatitis Alliance, alongside complete birth dose of hepatitis B vaccine and increase in treatment. Viral hepatitis can be diagnosed through assessing symptoms, a physical examination and also blood tests.
Tests for hepatitis B include: HBsAg positive, hepatitis B surface antibody, hepatitis B surface antigen and anti-HBs reactive. Delving into the THIN® data reveals 5,344 patients have at least one Hepatitis B Antibody test in THIN® - 63% of these are women; while 32,277 patients have at least one SH-antigen (hepatitis B) test in THIN®, 77% of these are women.
In the UK, alcoholic hepatitis, a type of hepatitis caused by drinking excessive amounts of alcohol over many years, is also common and, again often unrecognised by sufferers. Analysis of the THIN® database confirms that 62% of active patients with a diagnosis of hepatitis have at least one alcohol measurement in THIN®.
The World Hepatitis Alliance estimates that annual deaths will drop by 65% and 10 million lives will be saved by 2030 if countries meet a set of prevention and treatment targets. With the pressure facing health practitioners globally as a result of COVID-19, the use of epidemiological health data such as THIN® will play an important role in understanding progress identifying the missing millions with hepatitis, how prevention and treatment are being delivered and the implication on population health.
* Hepatitis includes patients with hepatitis A,B,C,E, hepatitis B with/without hepatitis D, chronic hepatitis and alcoholic hepatitis.
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.