Kidney health has declined during the COVID-19 pandemic
Three million people in the UK have chronic kidney disease (CKD) – and too often it is fatal. In 2019, five people died every week waiting for a kidney transplant. Sadly, the global pandemic has made the situation worse. Not only are people with CKD vulnerable and face a higher risk of becoming seriously ill or dying but the virus also affects kidney health: up to a quarter of people who have COVID-19 and receive ventilation in intensive care end up with severe acute kidney injury (AKI) and need dialysis.
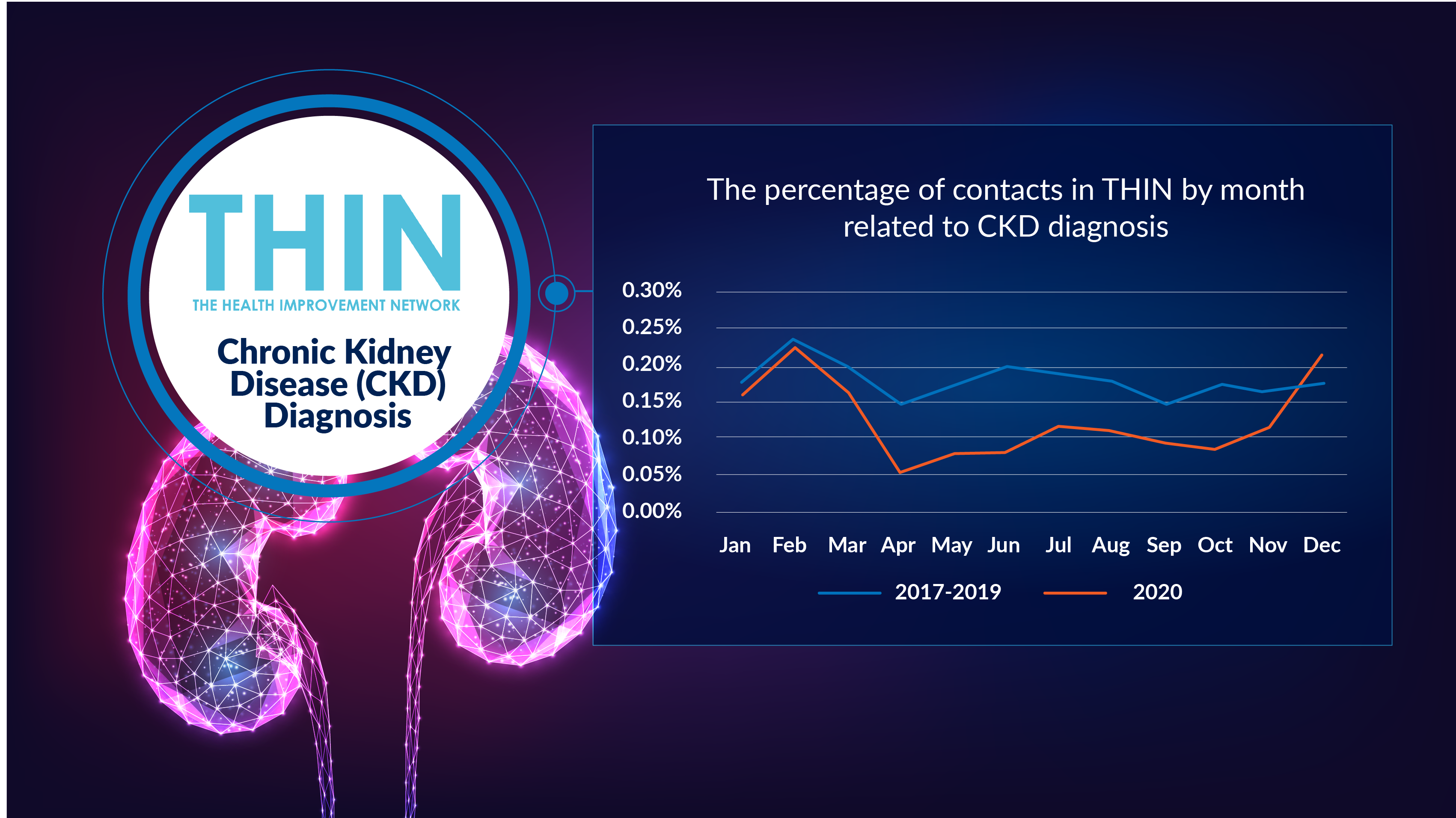
Furthermore, the triggers for CKD, including weight gain, lack of exercise, diabetes and hypertension, have increased during the pandemic – and the impact is clear. According to analysis of The Health Improvement Network (THIN®), a Cegedim database, while diagnosis of CKD dropped during lockdown, by the end of December 2020 CKD diagnoses actually surpassed baseline measures – something not seen in other disease areas, which are still below baseline.
Which is why the focus for this year’s World Kidney Day - The Big Topic everyone is ignoring – is spot on.
Kidney Health is Vital
Removing toxins, excess water and waste products, kidneys play a vital role in maintaining a healthy body - from regulating blood pressure to activating vitamin D. Yet according to figures from World Kidney Day, up to one million people in the UK may have undiagnosed CKD. Early diagnosis can have a significant impact on patient health and long term outcomes – treatment together with changes to diet and lifestyle can often help slow down or prevent any further damage. However, if CKD goes undetected or is not managed well, it can progress to kidney failure, which is fatal without treatment. Patients with kidney failure will need regular dialysis or a kidney transplant.
Factors that increase the risk of CKD include, diabetes, high blood pressure (hypertension) and heart and circulatory disease. A family history of kidney disease also needs to be taken into account, while a black, Asian or minority ethnic background could mean an increased risk of developing kidney failure more quickly. While these inherited conditions are not preventable they can be managed if diagnosed in time.
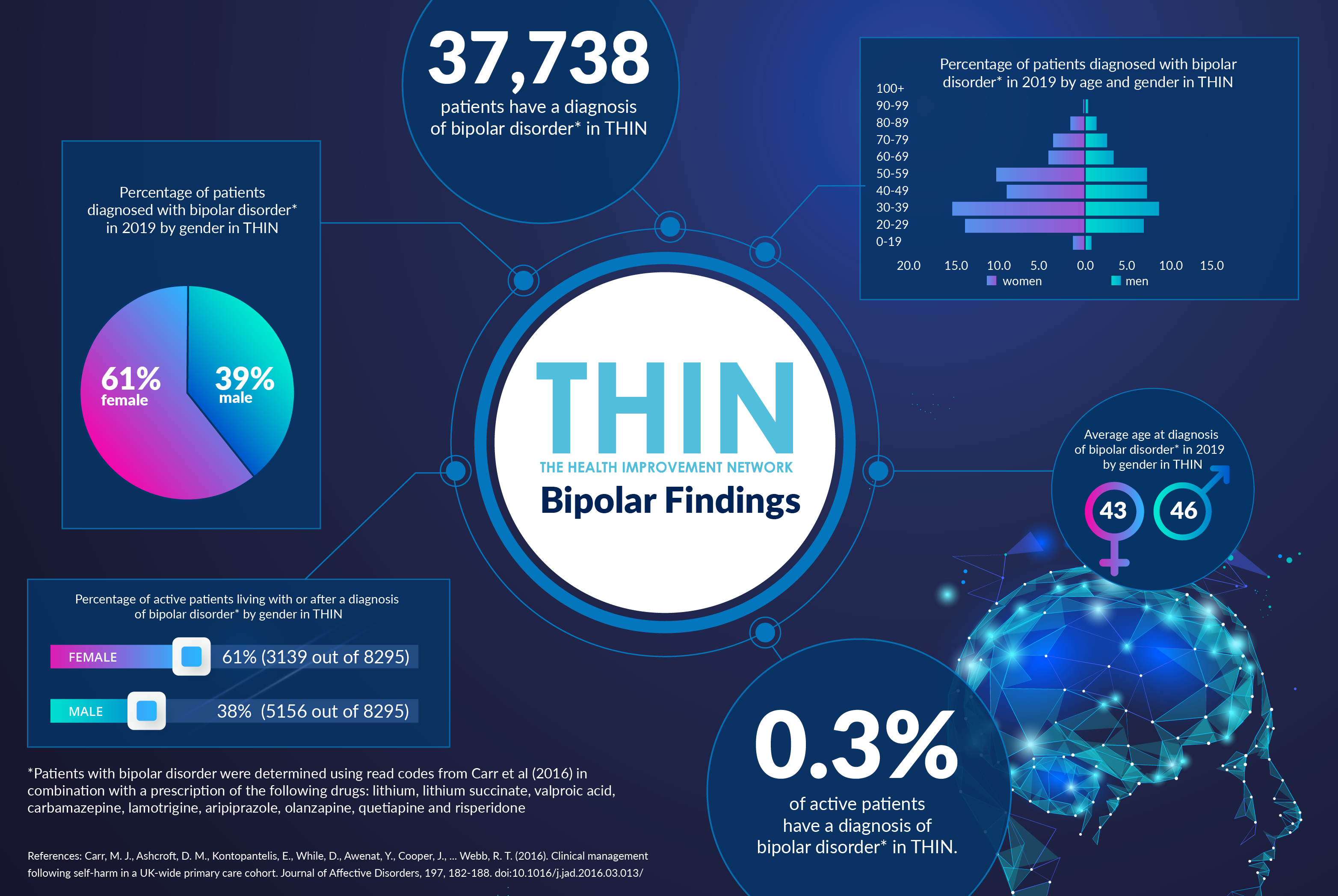
Analysis of THIN® data reveals more women (58%) are living with CKD than men (42%) – although the average age of diagnosis is 69 for both genders.
Understanding Comorbidities

The impact of comorbidities on CKD is confirmed by analysis of THIN® data: two thirds (67%) of patients with a diagnosis of CKD also have a diagnosis of hypertension. In addition, 28% of patients with a diagnosis of CKD also have a diagnosis of heart failure, 22% coronary heart disease and 14% asthma.
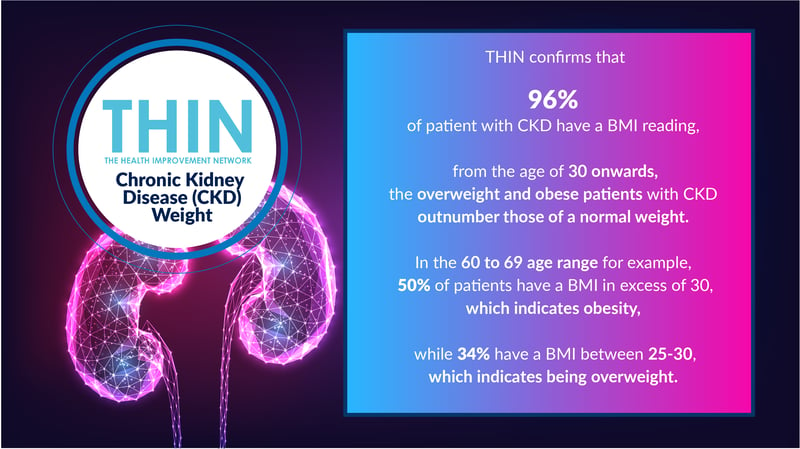
Patients with CKD are also overweight and obese. THIN® confirms that 96% of patient with CKD have a BMI reading, and from the age of 30 onwards, the overweight and obese patients with CKD outnumber those of a normal weight. In the 60 to 69 age range for example, 50% of patients have a BMI in excess of 30, which indicates obesity, while 34% aged 60 to 69 have a BMI between 25 and 30, which indicates being overweight.
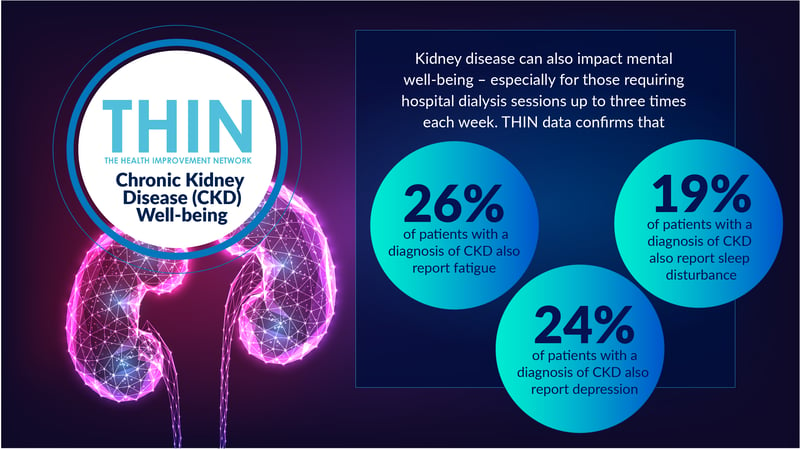
Kidney disease can also impact mental well-being – especially for those requiring hospital dialysis sessions up to three times each week. THIN® data confirms that 26% of patients with a diagnosis of CKD also report fatigue, 24% depression, and 19% sleep disturbance. Almost a quarter (22%) also report oedema - swelling caused due to excess fluid accumulation in the body tissue, which can be life limiting by restricting movement.
Pandemic Impact
The pandemic has badly impacted kidney patients, with many having to shield at home for the past year. Dialysis patients, however, have been compelled to visit hospital several times a week for their life-saving treatment. And those with a kidney transplant or taking immunosuppressants still have to attend their regular medical appointments, despite being less able to fight the virus because of the drugs they take.
The pandemic has also led to more people with otherwise healthy kidneys to develop problems – from the AKI associated with severe COVID-19 requiring ventilation to the escalation in hypertension, weight gain and diabetes that has occurred during the past 12 months. During the COVID-19 pandemic, over a third of UK adults confess to having gained weight, while the stress and social isolation of repeated lockdowns is believed to cause an increase an high blood pressure.
This is putting ever greater pressure on clinicians to rapidly identify those at risk of CKD and put in place the treatment and lifestyle change regimes required to minimise the risk of problems escalating.
Assessing Kidney Health
Kidney health is typically assessed through a glomerular filtration rate (GFR) test which estimates how much blood passes through the glomeruli - the tiny filters in the kidneys that filter waste from the blood – each minute.
In addition, a simple urine test checks for blood or albumin (a type of protein) in the urine – both of which can be an early sign of kidney disease. THIN® data confirms that 94% of active patients with CKD have at least one albumin test result and 97% of active patients with CKD have at least one glomerular filtration rate test result.
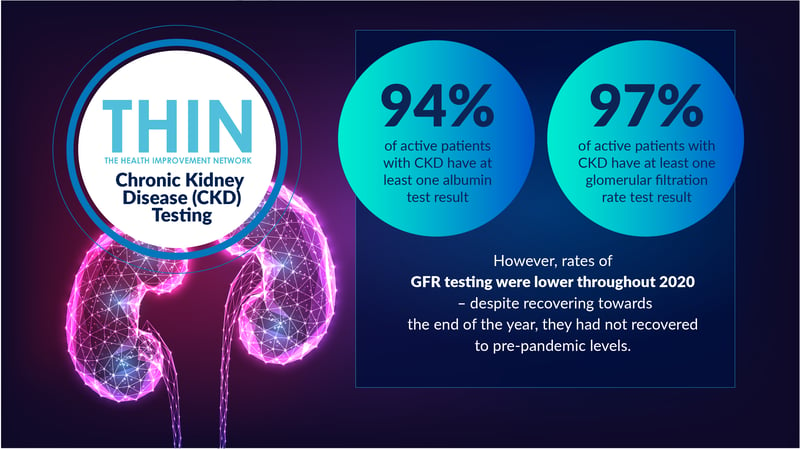
However, rates of GFR testing were lower throughout 2020 – despite recovering towards the end of the year, they had not recovered to pre-pandemic levels, raising further concerns regarding undiagnosed CKD.
This is where anonymised longitudinal data resources such as THIN® are providing a vital support for clinicians managing post-pandemic health challenges. Improved understanding of population health can help to identify those at risk of CKD, understand trends in diagnosis and support targeted wellbeing programmes to encourage the lifestyle interventions that can play a vital role in minimising the risk of CKD and improving kidney health.