Highlighting Stress Related Behaviour Changes in Stress Awareness Month
2020 has had a devastating effect on many individual’s physical and mental well-being: new research from the Mental Health Foundation states that 74% of UK adults in the past year have felt overwhelmed or unable to cope as a result of stress.
According to the Stress Management Society, stress is one of the great public health challenges of our time – yet still isn’t being taken as seriously as physical health concerns. Stress is a significant factor in mental health problems including anxiety and depression. It is also linked to physical health problems like heart disease, problems with our immune system, insomnia and digestive problems.
Individuals can take action to address stress – starting with understanding what is causing personal stress and then learning the steps that can be taken to reduce that stress. Which is why this year’s theme for Stress Awareness Month 2021 is ‘Regaining Connectivity, Certainty and Control’.
Changing Behaviours
Recent research from the Stress Management Society identified that 65% of people in the UK have felt more stressed since the COVID-19 restrictions began in March 2020 – and the three key causes for concern are feelings of disconnection, uncertainty, and a worrying loss of control. Typical physical symptoms of stress include heart palpitations, dry mouth, headaches, dizziness, nausea, tiredness & insomnia, a change in eating habits and sudden weight loss or gain.
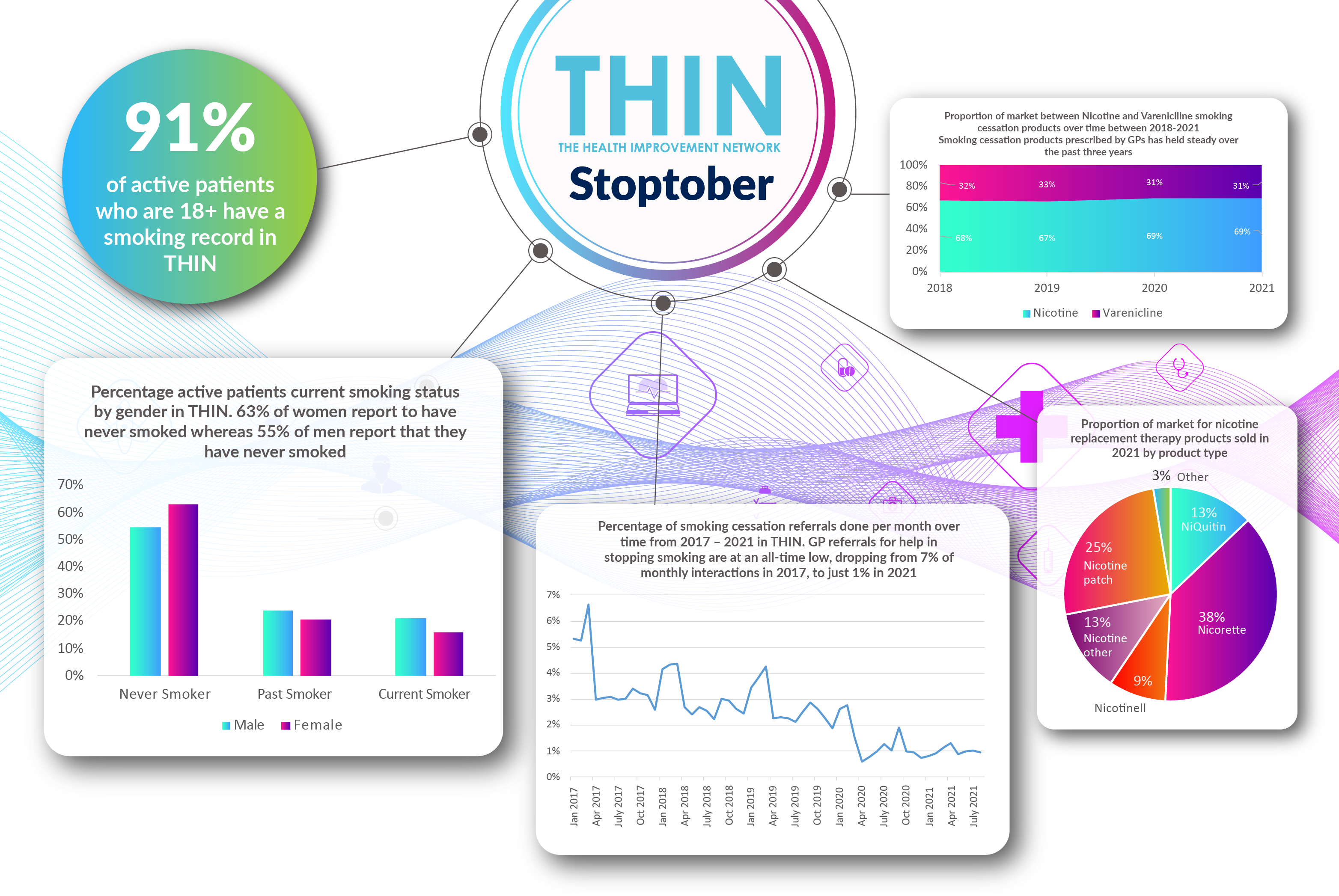
Behavioural changes can include nail biting and bad temper but it is also concerning to discover the way many individuals have responded to pandemic related stress. The latest research from Mintel suggests the stress of COVID-19 has fuelled Britain’s smoking habit: over half (51%) of smokers are stress-smoking more since the beginning of the pandemic.
While the pandemic is shining a spotlight on the nation’s health concerns, young smokers in particular are turning to vices, as 39% of smokers aged 18-34 say they are now smoking more regularly. Meanwhile, a further 10% of all smokers have started smoking again after quitting. Overall, 30% of smokers are smoking more regularly since the start of the pandemic. And it’s not just smoking which has seen increases; more than four in 10 (42%) e-cigarette users are vaping more regularly too.
Cardiovascular Disease
While smoking is increasing, the survey also confirms that two thirds (65%) of Britain’s smokers acknowledge they are worried that the virus is more dangerous to them as a smoker. A further seven in 10 (69%) say that their respiratory health is more important to them now than before the COVID-19 outbreak.
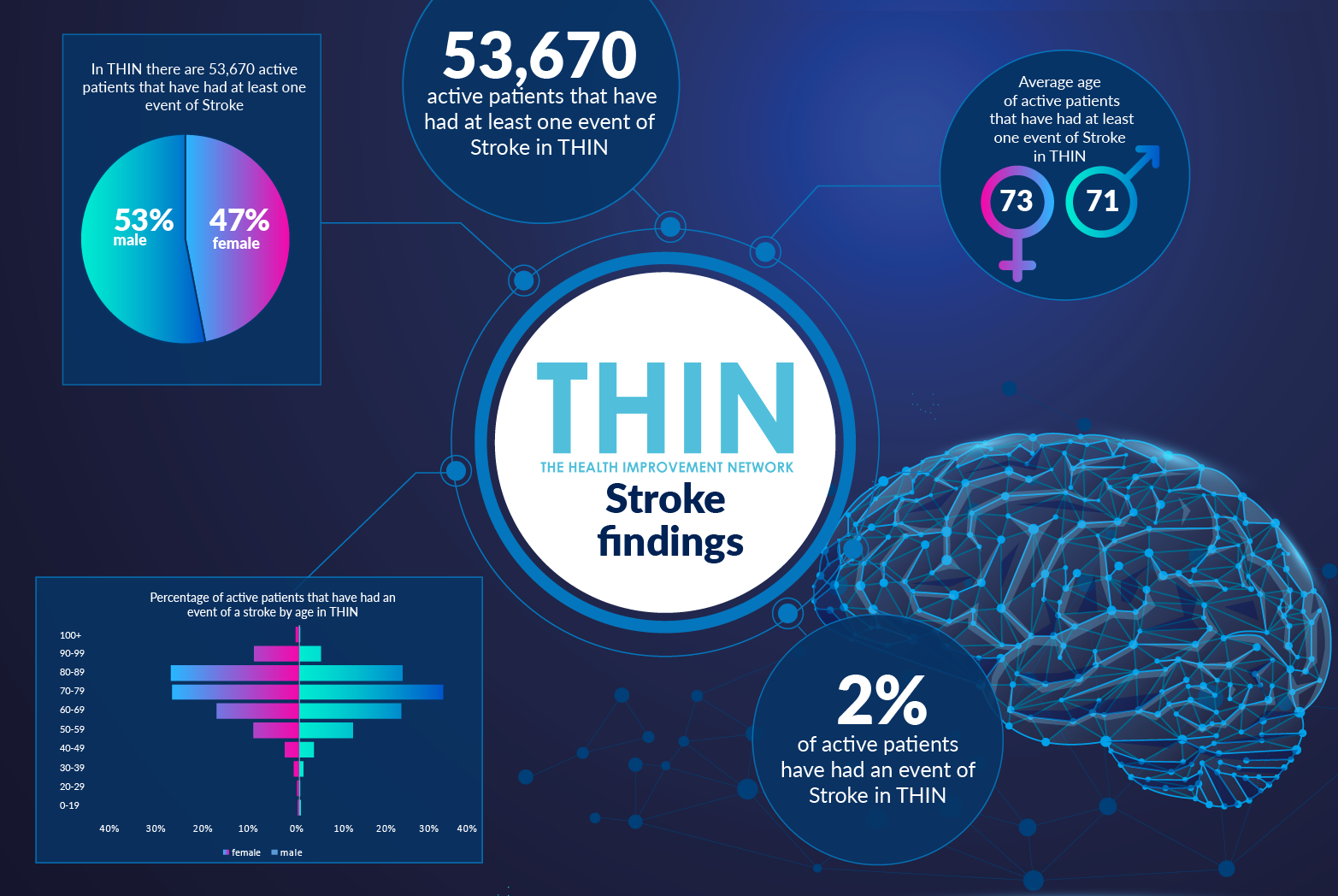
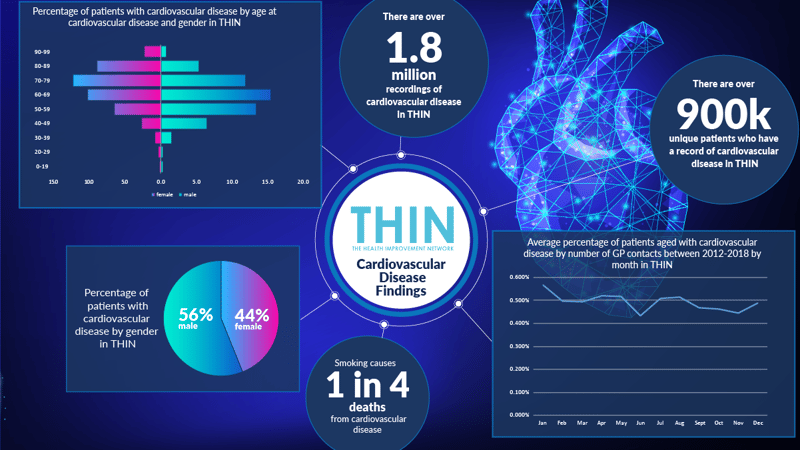
However, both stress and smoking are significant co-morbidities for cardiovascular disease (CVD), creating additional concerns for health care practitioners. The scale of CVD in the UK is already creating a serious burden on the NHS. The Health Improvement Network (THIN®), a Cegedim database, is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. Analysis of the database reveals over 900,000 unique patients already diagnosed with CVD – 44% female, 56% male. With smoking causing one in every four deaths from CVD, this stress related increase in smoking, especially across the younger population, is a serious concern for health care professionals.
Panic and Pain
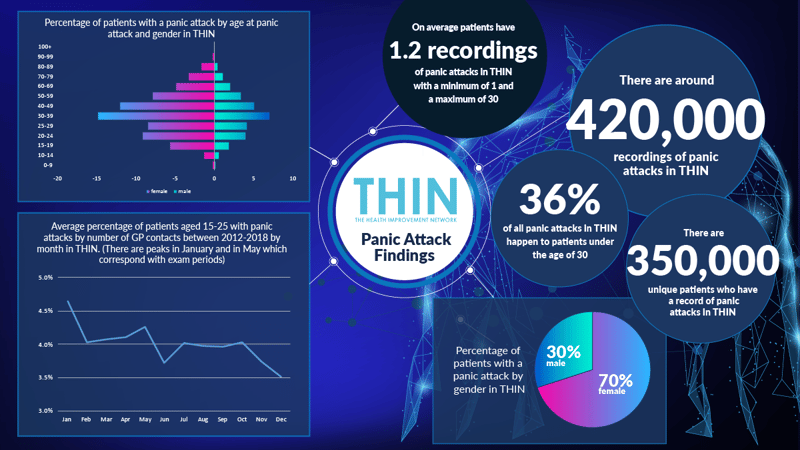
In addition to negative behavioural changes, stress can manifest in many ways, from debilitating panic attacks to headaches. Analysis of THIN® reveals that panic attacks affect women (70%) more than men (30%). There are over 420,000 recordings of panic attacks in THIN® – associated with 350,000 unique patients. The panic attacks affect the young more than the old – 36% are experienced by individuals under 30, while the percentage of GP contacts for panic attacks for those aged between 15 and 25 peaks during exam periods in January and May.
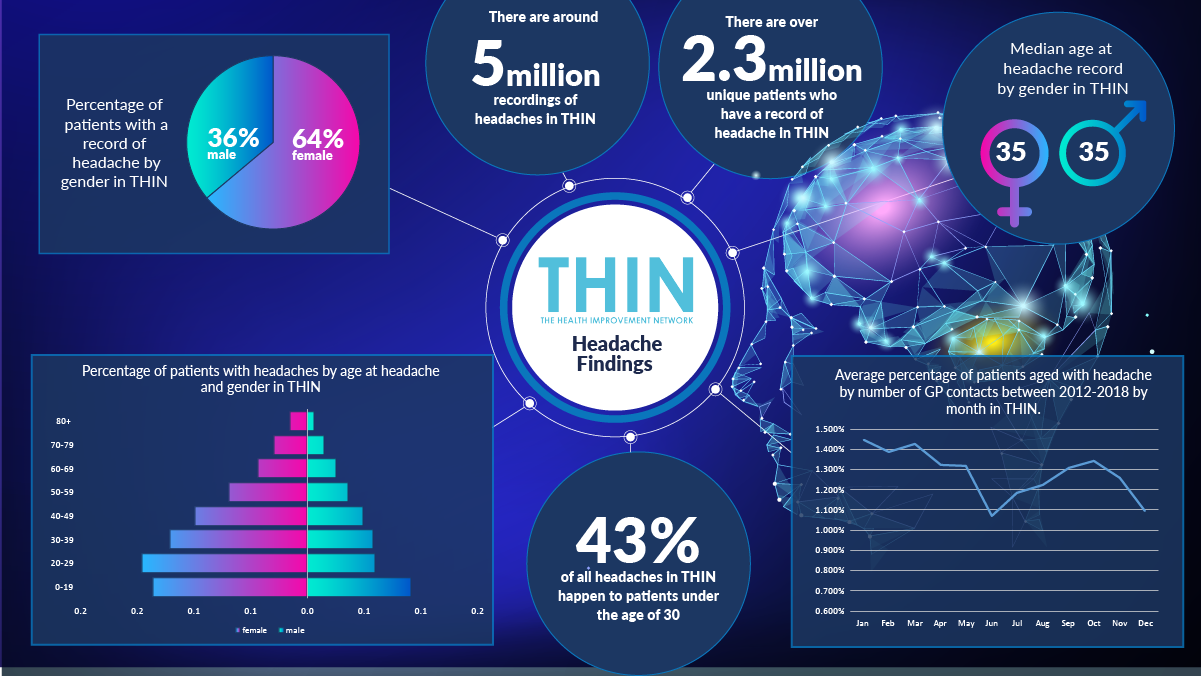
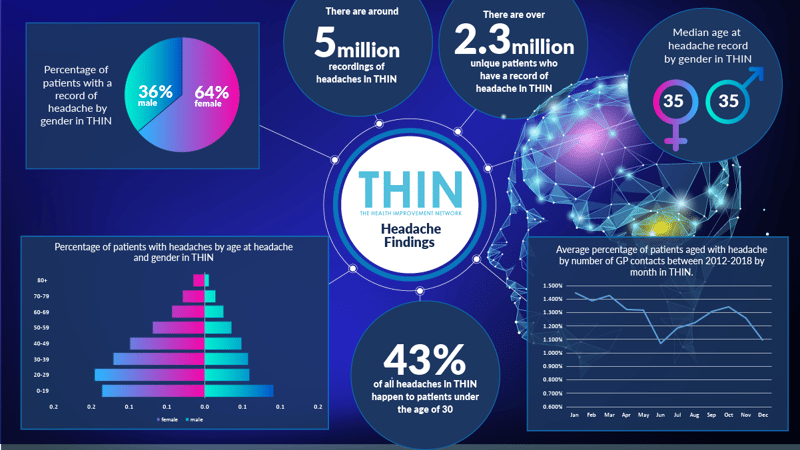
Headaches are also a significant concern, especially for younger generations. THIN® data confirms 2.3 million unique patients with a record of a headache – 64% are female, 36% male – and 43% of headaches in THIN® occur to patients under the age of 30. Managing patients with headache demands a significant portion of GP time – with as many as 1.45% of GP contacts comprising patients with headache.
Empowering Individuals with Lifestyle Change
Of course, individuals can be supported to achieve better stress management, reducing their reliance on health care practitioners and improving their long term outcomes. The Mental Health Foundation suggests three steps that can be taken when feeling stressed: notice the problem; identify the causes and review your lifestyle.
Additional changes including healthy eating, reducing smoking and alcohol consumption, increasing exercise, taking time out, adding mindfulness and improving sleep. Many primary care services are already offering a range of services to support such lifestyle changes – such as the use of Health Coaches to support a long term overhaul in behaviour.
But it will also be important to understand the impact of this extraordinary pandemic related stress on the population at large – from the learning disruption affecting school age children to financial worries, and the isolation of the elderly and shielding.
Population Strategies to Combat Stress
Furthermore, in addition to the grief and isolation that has been experienced, many of the significant changes that have occurred over the past year, such as working from home, are now set to remain in place – and that will need new coping mechanisms for many. Financial worries and job security are issues that individuals will need to deal with for months, even years, to come – however successful the COVID-19 mitigation strategies may be.
Given the unprecedented backlog in patients waiting for treatment across the NHS, there is little room to support this additional wave of stress related problems – and there will be a need to find new ways to identify and support individuals in managing stress. This is where population health data such as THIN® is so vital – not only in highlighting trends in patient concerns that might reveal intolerable levels of stress but also in tracking stress mitigation programmes within the community and understanding how different activities, such as social prescribing and health coaching, are working to provide vital support.