International Day of People with Disabilities
On December 3rd this year, during the annual celebration of people with disabilities, the 2020 theme ‘Not all Disabilities are Visible’ also focuses on spreading awareness and understanding of disabilities that are not immediately apparent, such as mental illness, chronic pain or fatigue, sight or hearing impairments, diabetes, brain injuries, neurological disorders, learning differences and cognitive dysfunctions, among others.
During the COVID-19 pandemic, isolation, disconnect, disrupted routines and diminished services have greatly impacted the lives and mental well-being of people with disabilities right around the world. Spreading awareness of invisible disabilities, as well as these potentially detrimental— and not always immediately apparent— impacts to mental health, is crucial as the world continues to fight against the virus.
Living with Disability
According to the WHO World Report on Disability, 15 per cent of the world’s population, or more than 1 billion people, are living with disability. Of this number, it’s estimated 450 million are living with a mental or neurological condition— and two-thirds of these people will not seek professional medical help, largely due to stigma, discrimination and neglect. Another 69 million individuals are estimated to sustain Traumatic Brain Injuries each year worldwide, while one in 160 children are identified as on the autism spectrum.
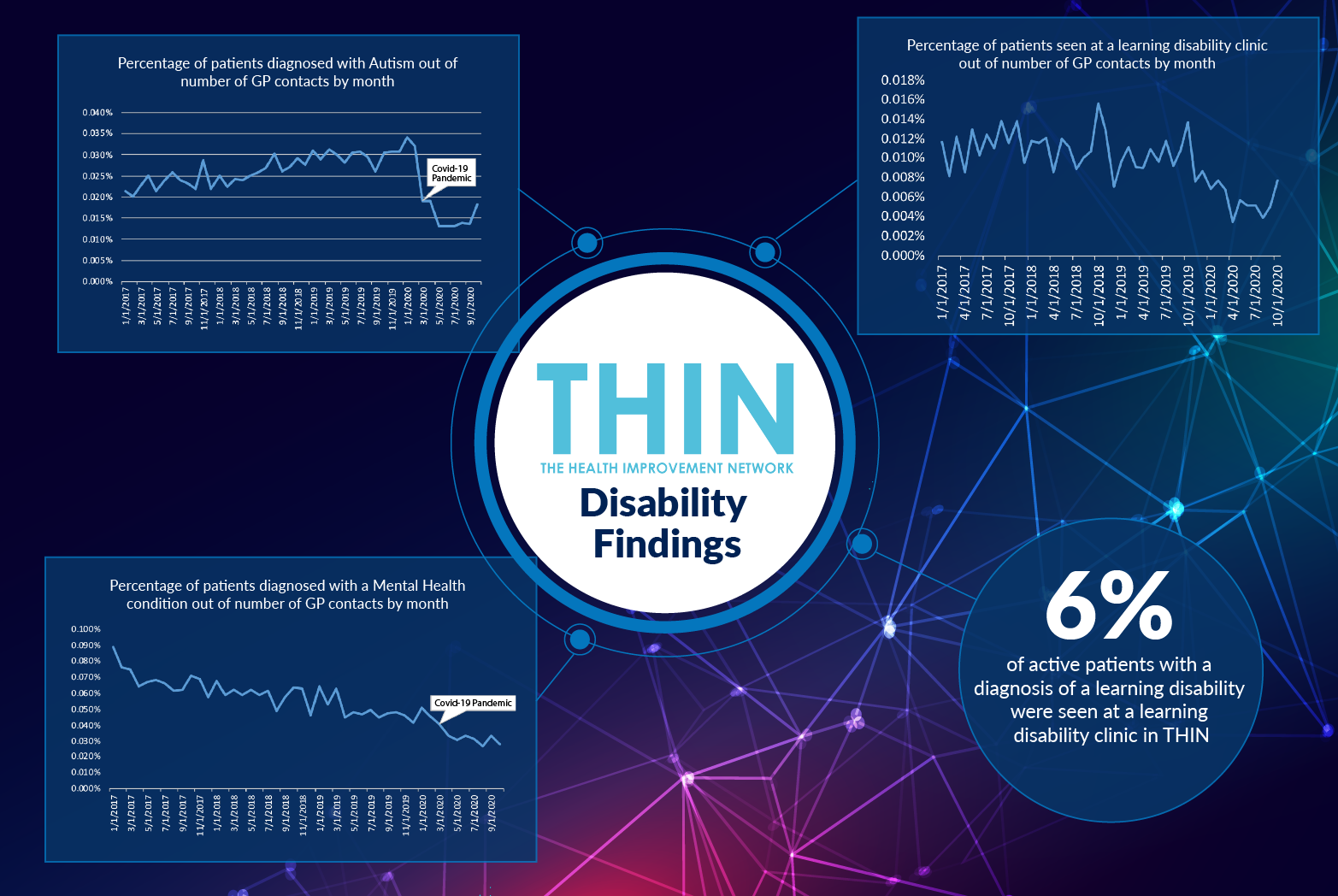
The implications of people failing to seek professional help has come into sharp focus during the COVID-19 pandemic. Yet as analysis of The Health Improvement Network (THIN®), a Cegedim database, confirms trends in mental health diagnosis have been heading downwards for some time – despite the rise in individuals reporting mental health issues.
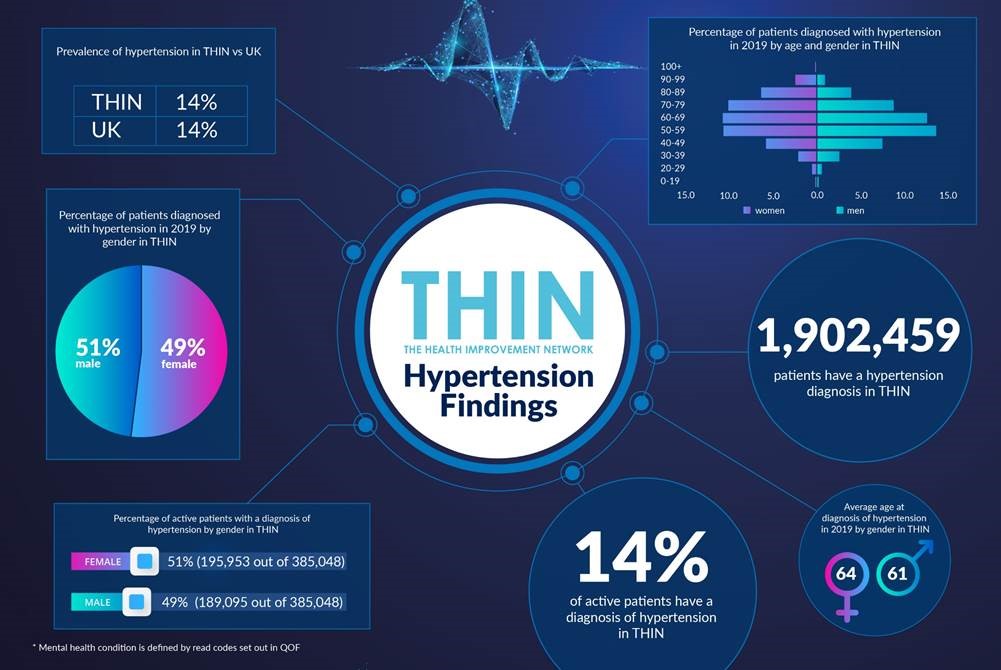
According to THIN®, of the total number of GP contacts, the percentage of patients diagnosed with all mental health conditions has fallen year on year since the beginning of 2017 – and has dropped even further during the COVID-19 pandemic to around a quarter of levels four years ago. The percentage of patients with a referral for a mental health clinic or counsellor out of number of GP contacts by month has also dropped; while just 6% of active patients with a diagnosis of a learning disability were seen at a learning disability clinic in THIN®.
The impact of the pandemic has been particularly devastating for certain life-limiting conditions. By May 2020 autism diagnoses, for example, had fallen to one third of the levels at the beginning of the year; while Chronic Fatigue Syndrome (CFS) diagnoses had fallen to one quarter of January 2020 levels.
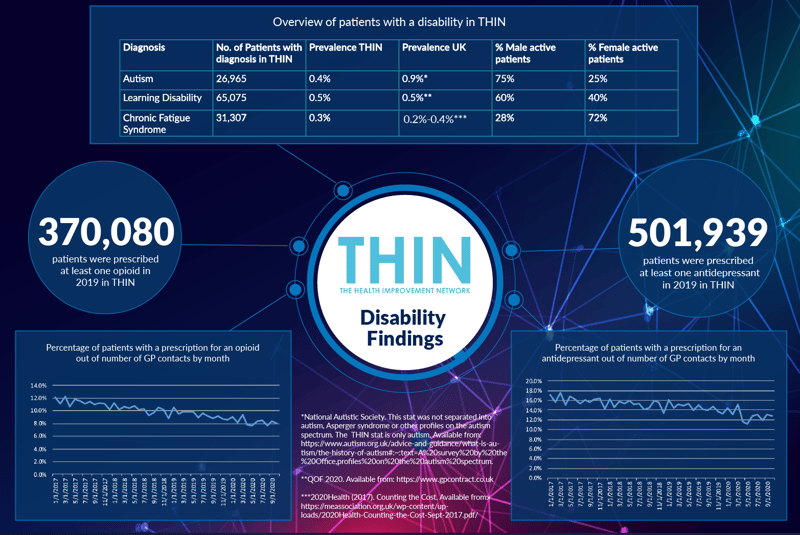
Recognising Gender Difference
Male and female patients have very different patterns of diagnosis with regards to disabling conditions. For example, of the 26,965 patients with a diagnosis of Autism in THIN®, three quarters (75%) are male. This condition is typically diagnosed young; the vast majority of individuals received a diagnosis under the age of 15. Males are also more likely to be diagnosed with a learning disability – of the 65,075 patients with a diagnosis of a learning disability in THIN®, 60% are men. Again the age of diagnosis is relatively young, under 30.
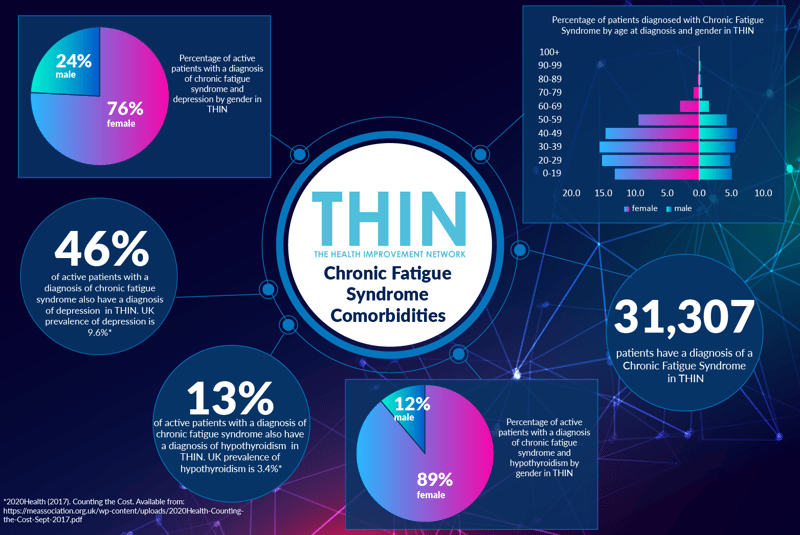
In contrast, women are far more likely to be diagnosed with CFS than men. Of the 31,307 patients with a diagnosis of CFS in THIN®, almost three quarters (72%) are female. Individuals are susceptible to CFS at any age, although diagnosis drops off significantly after the age of 50 for both men and women.
In addition to revealing trends in GP contacts and referrals, THIN® data has also surfaced changes to prescribing trends in recent years. 370,080 patients were prescribed at least one opioid, for pain relief, in 2019 and 501,939 patients were prescribed at least one antidepressant in 2019 in THIN®. However, opioid prescriptions fell from 12% of GP contacts in January 2017 to 8% in September 2020; while antidepressant prescriptions fell from 17% of GP contacts in January 2017 to 13% in September 2020 – in both cases, the trend predates the COVID-19 pandemic.
Female patients of all ages are far more likely to receive prescriptions for both opioids and antidepressants than male patients – although for all genders, people aged between 50 and 59 are more likely to receive an antidepressant prescription.
Understanding Comorbidities
THIN® analysis also confirms a number of CFS comorbidities that will affect day to day living – not least that almost half (46%) of all active patients with a diagnosis of CFS also have a diagnosis of depression in THIN®, far higher than the 9.6% UK prevalence of depression. 13% of active patients with a diagnosis of CFS also have a diagnosis of hypothyroidism in THIN® – compared to the UK prevalence of hypothyroidism at 3.4%. This comorbidity particularly affects women (89%).
Other comorbidities to note include the level of hypertension for patients with a diagnosis of Parkinson’s. THIN® data reveals over half 59% of active patients with a diagnosis of Parkinson’s also have a diagnosis of hypertension in THIN® – compared to the UK prevalence of hypertension of 14.1%. Again this comorbidity primarily affects women (89%).
This is an interesting discovery given the debate regarding hypertension and Parkinson’s disease. The population study: “Association between Hypertension and the Risk of Parkinson’s Disease: A Meta-Analysis of Analytical Studies,” suggests a link between hypertension and greater prevalence of Parkinson’s. However, Parkinson’s patients often suffer hypotension – and one recent study has suggested a simple bedside test measuring heart rate and blood pressure after a patient stands may help doctors come up with an early diagnosis of Parkinson’s and other neurodegenerative disorders.
Another notable difference in the way men and women experience disability is in the comorbidity of diabetes and Schizophrenia - 89% of the active patients with a diagnosis of both schizophrenia and diabetes in THIN® are female.
Focusing Post-COVID Care
We know that COVID-19 has had an impact on the mental health of many individuals – and with major depression thought to be the second leading cause of disability worldwide and a major contributor to the burden of suicide and ischemic heart disease* this is a situation that needs carefully monitoring. With so much pressure on clinicians in both primary and secondary care, THIN® data can provide vital insights – not least in helping to identify those individuals failing to request professional help when needed, and specifically highlighting the potentially different experiences of male and female patients.
With the rise in long COVID patients, many of whom are experiencing disabling conditions, from pain to fatigue and depression, also appearing to affect women more than men, further focus on gender differences is set to play a vital role in tailoring care strategies.
*Whiteford, H. A. et al. (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010
About THIN®
THIN® is an unobtrusive medical data collection scheme that contains anonymised longitudinal patient records for approximately 6% of the UK population. It is the key driving force behind enabling advancements in patient care and outcomes, with one of the most respected and reliable data sources for anonymised primary care records.