Prioritising Invitations in Delayed Screening Programmes
Screening programmes have become a core strand within NHS disease prevention strategies over recent years – with cervical screening one of the most far reaching. Every year five million women and people with a cervix are invited for screening – and the screening process can prevent up to 75% of instances of cervical cancer, saving 5,000 deaths per year.
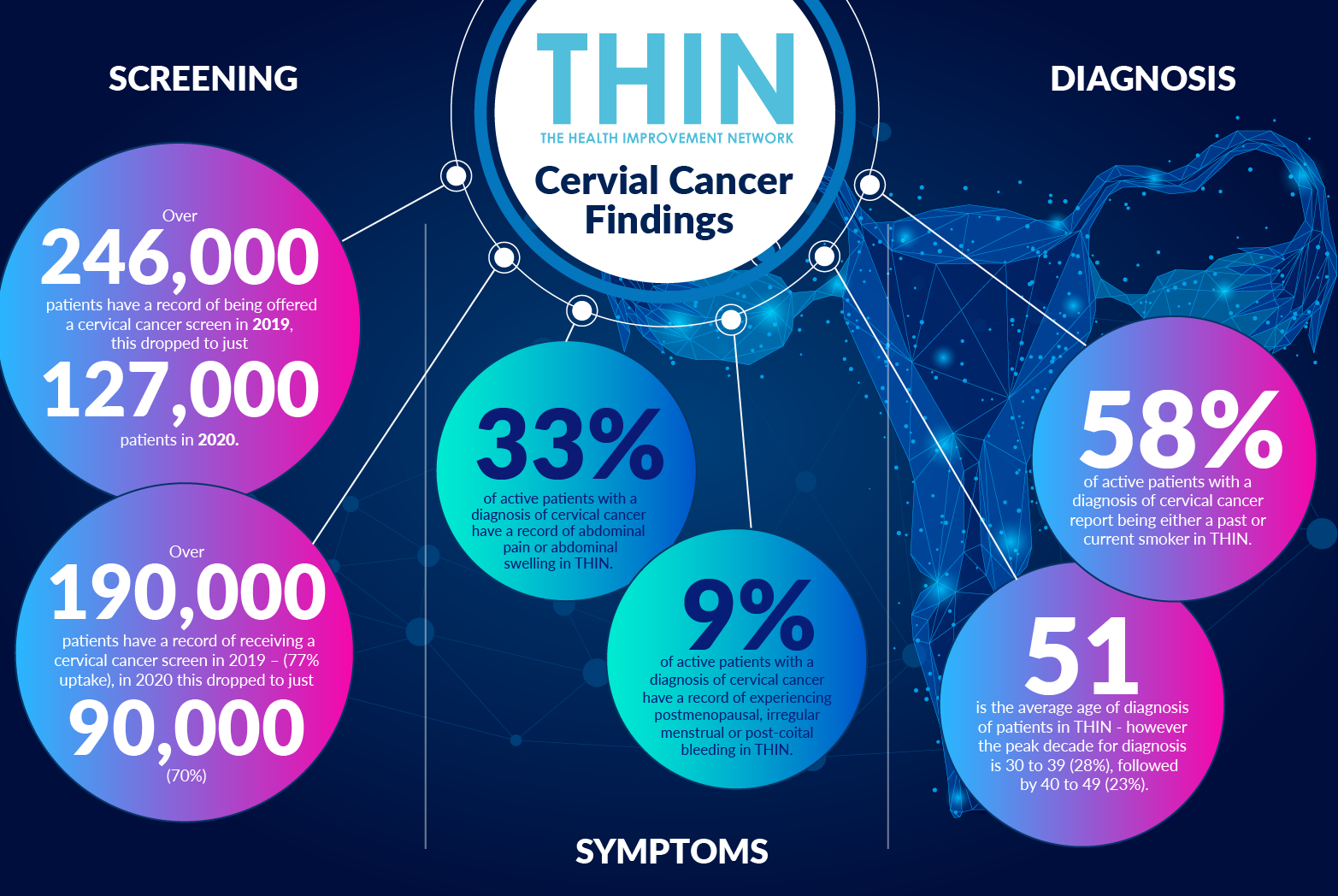
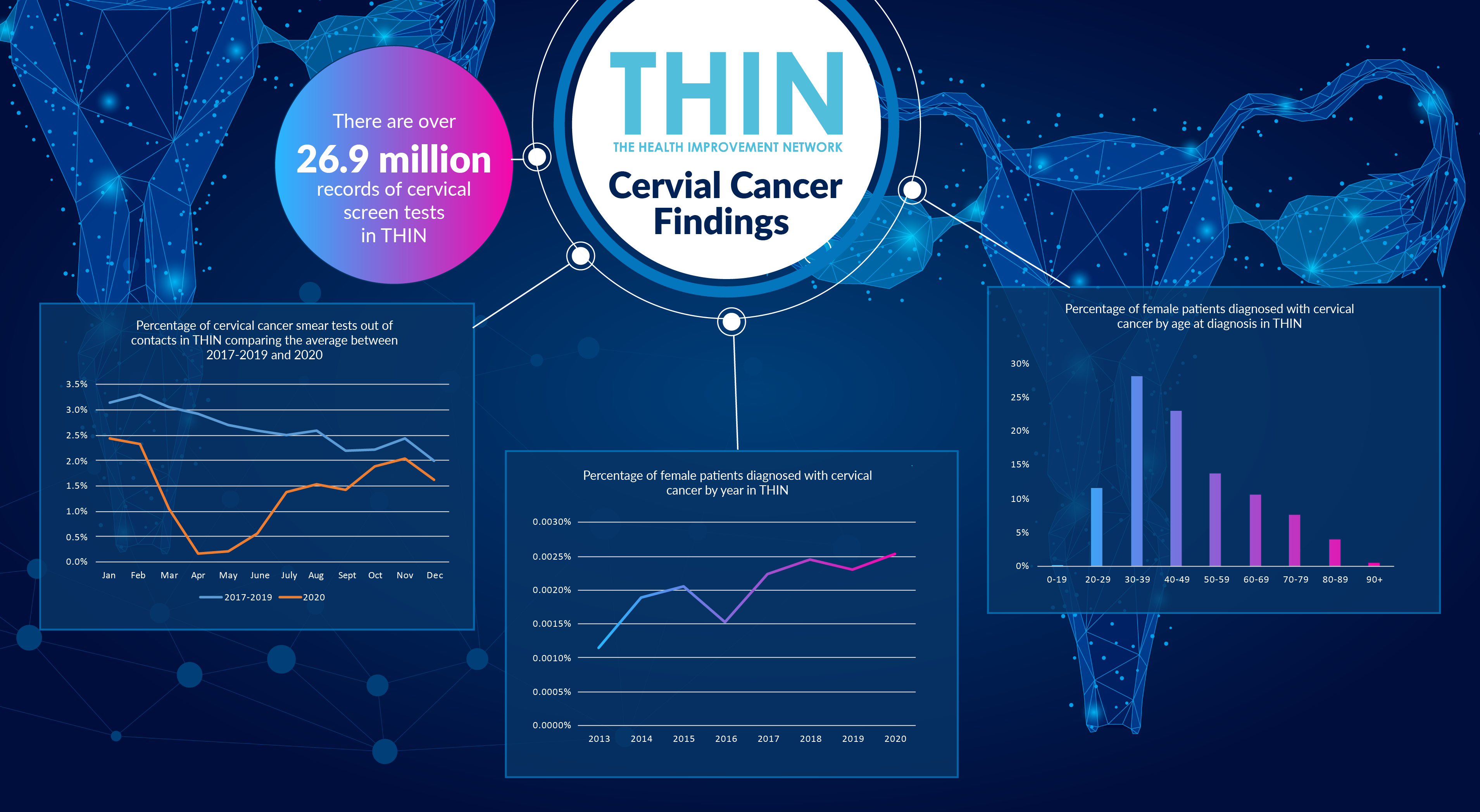
However, in common with many routine screening activities, the numbers invited to and attending cervical screening during 2020 dropped. Analysis of The Health Improvement Network (THIN®) a Cegedim database, revealed the percentage of cervical cancer smear tests out of contacts were significantly down in 2020 compared to the average between 2017 and 2019. The numbers plummeted in March 2020 when all non-urgent activity was suspended and very few tests occurred in April or May 2020. However, a year on and attendance for cervical cancer screening has now increased and is now back to pre-pandemic levels.
This year’s Cervical Screening Awareness Week, an annual event which runs from 15th to 21st June 2021, which aims to highlight the importance of regular cervical screening for women’s health has never been more important.
Overcoming Reluctance
Despite the proven benefits of cervical screening, many women are reluctant to have this test. Even before COVID-19 induced delays, as many as one quarter of women failed to respond to their screening invitation, according to the charity Jo’s trust, which is dedicated to women affected by cervical cancer or anomalies.
Recent research by the charity into reasons for non-attendance confirmed that in addition to the pre-pandemic barriers and motivators to attendance – such as fear, embarrassment, pain or discomfort, or inconvenience - many women either have concerns regarding NHS capacity or simply assume screening is not happening.
In addition, there is a misperception that the Human Papilloma virus (HPV) vaccination, introduced in 2008 for adolescent girls in secondary school, eradicates the need for screening. HPV is associated with 99% of cervical cancer diagnoses – and over 460,000 patients had at least one HPV vaccine in THIN®. However, while the vaccine is playing a key role in reducing the incidence of cervical cancer, as the NHS guidance confirms, the HPV vaccine does not protect from all types of HPV.
Rising Risk
Despite the extensive vaccination programme, the incidence of cervical cancer is rising. This is primarily within age groups that had left school before the vaccine was introduced plus, of course, with the number of people getting cervical cancer tests rising, more cancers are being diagnosed. Analysis confirms over 12,000 patients have a diagnosis of cervical cancer in THIN® and the number of patients diagnosed by year doubled between 2013 and 2020.
Women are most likely to be diagnosed with cervical cancer between the ages of 30 and 39 (28%) or 40 and 49 (23%), according to THIN® data. Analysis also confirms that a third of the 14,000 patients with a diagnosis of HPV in THIN® are aged between 20 and 29, while 35% are aged between 30 and 39.
This peak in diagnoses between 30 and 49 supports the current NHS policy of inviting women for screening as they approach their 25th birthday, with follow up tests every three years until 50 – at which point the frequency is reduced to every five years.
Reinvigorating Screening Programme
THIN® analysis confirms the extent of cervical screening undertaken to date: over 4.7 million female patients had at least one cervical cancer screen in THIN®, and the database includes over 26.9 million records of cervical screen tests.
The delays due to the COVID-19 pandemic are particularly concerning because in December 2019, the NHS introduced a more sensitive cervical screening test as part of the NHS Long Term Plan. The new test now looks for traces of 14 high risk HPVs which cause nearly all cases of cervical cancer and any tests that are HPV positive are then checked for abnormal changes of the cervix. The NHS believes the new test will identify far more cases, earlier, saving hundreds of lives and, in conjunction with the HPV vaccine, potentially eliminating the cancer.
The importance of more sensitive tests cannot be underestimated as cervical cancer may not cause any symptoms – or the symptoms may not be obvious. Common symptoms can include vaginal bleeding that is unusual for an individual patient, including after the menopause, after sex, or between regular periods; changes to vaginal discharge; pain or discomfort during sex and unexplained pain in the lower back or pelvis.
Self-Sampling
In addition to the more sensitive test, there is also a move to offer women the opportunity to self-sample. This approach enables women to collect their own sample for cervical screening using a vaginal swab or brush, and the self-samples are analysed for the presence of the human papillomavirus (HPV).
Self-sampling has already been integrated into the national screening programmes of The Netherlands, Denmark, Australia and Malaysia and offers a number of benefits - from the ease and privacy of self-sampling helping to overcome reluctance to freeing up clinician time. However, some patients are concerned about not correctly taking the sample, having greater confidence in trained professional and the risk of procrastination – making appointment for screening is making commitment to it happening.
According to Jo’s trust, women were split on their preferences between being sent a kit to take a sample at home using a vaginal swab (32%) compared to the usual cervical screening (smear test) with a doctor or nurse (31%). However, women who rarely or never book a test or have opted out of screening in the past are far more likely to prefer self-testing (47%) than clinician-led screening (9%). The same is true for women who are overdue, with 50% preferring a self-test and 18% preferring clinician-led screening.
Given the number of women who missed a cervical screening test in 2020, adding self-sampling to the programme could be a vital step in catching up the backlog. Since January 2021, a number of GP practices across North Central and North East London have been taking part in the YouScreen study, offering HPV self-sampling to non-attenders within the NHS Cervical Screening Programme (NHS CSP). YouScreen integrates self-sampling into the NHS CSP for the first time and will help provide the evidence base for this approach to cervical screening.
This is where population health data such as THIN® can provide vital insights – from helping to identify those individuals who have missed a routine test to those who consistently opt out and could be ideal candidates for self-sampling. As the NHS looks at innovative ways to address the backlog across all disease areas, finding ways to reinvigorate key preventative strategies, such as screening, could become ever more important. Rapid analysis of population health data to understand the uptake of screening – both in practice and self-sampling – the success rates and patient outcomes will help refine strategies to support both patient needs and clinical resources.