More to Cholesterol than Statins
Everyone needs some cholesterol, but according to Heart UK over half of UK adults have raised cholesterol, which can lead to heart disease. For many individuals, positive lifestyle changes can make a difference and keep cholesterol levels healthy. But there are other factors that can affect cholesterol levels – including genetics and menopause – and, left unchecked high cholesterol (hypercholesterolemia) may lead to atherosclerosis (the deposition of cholesterol in the walls of arteries) which can reduce the flow of blood to the heart and brain, leading to heart diseases and stroke.
Globally, nations have adopted preventative strategies to mitigate the risk of high cholesterol; in the UK alone over eight million people are routinely prescribed cholesterol lowering drugs (Statins). Given the significant population groups both with high cholesterol and taking prescribed medication it is therefore vital not only for individuals to understand – and check – their cholesterol levels but also for clinicians to understand and track the efficacy of both lifestyle change and medication.
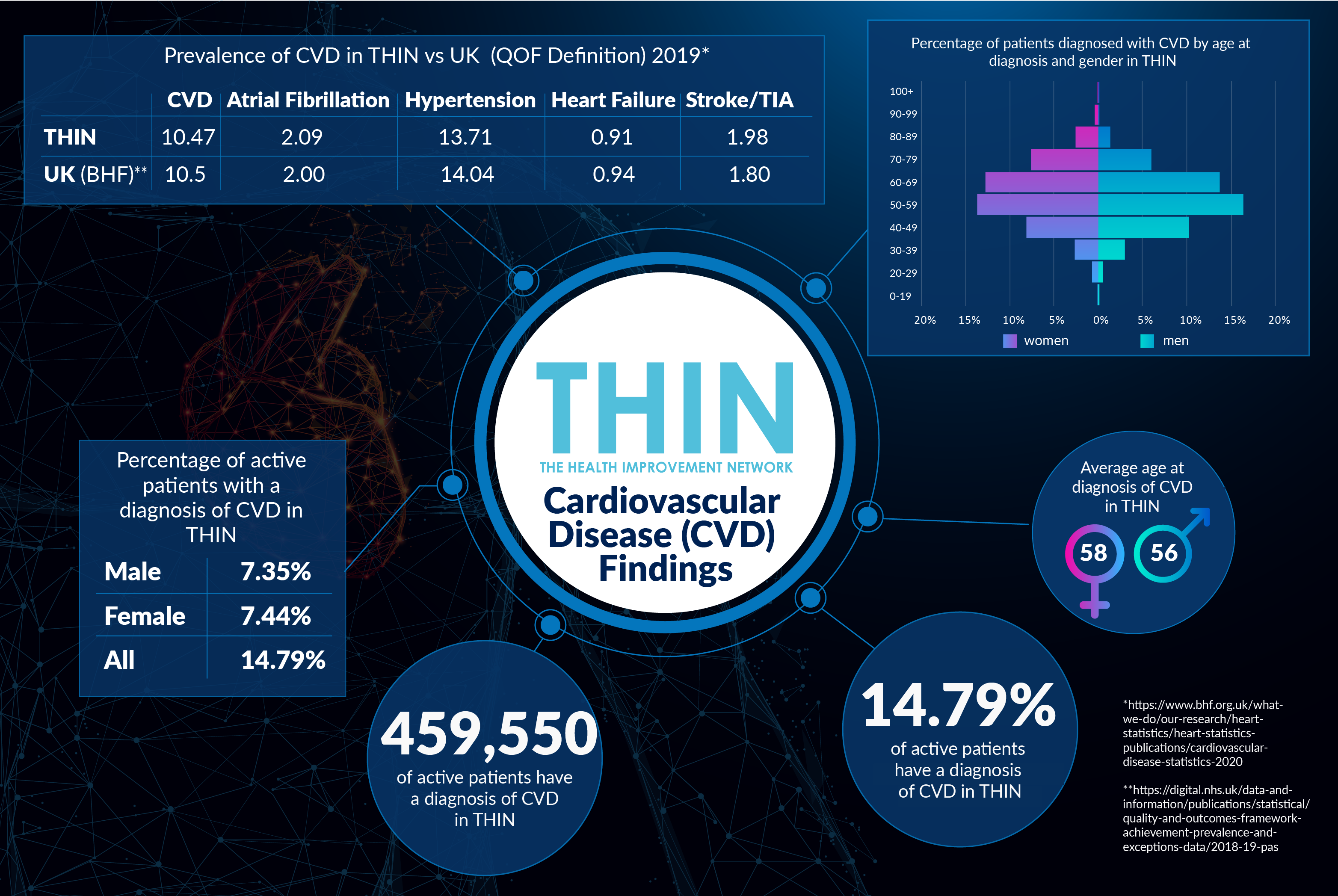
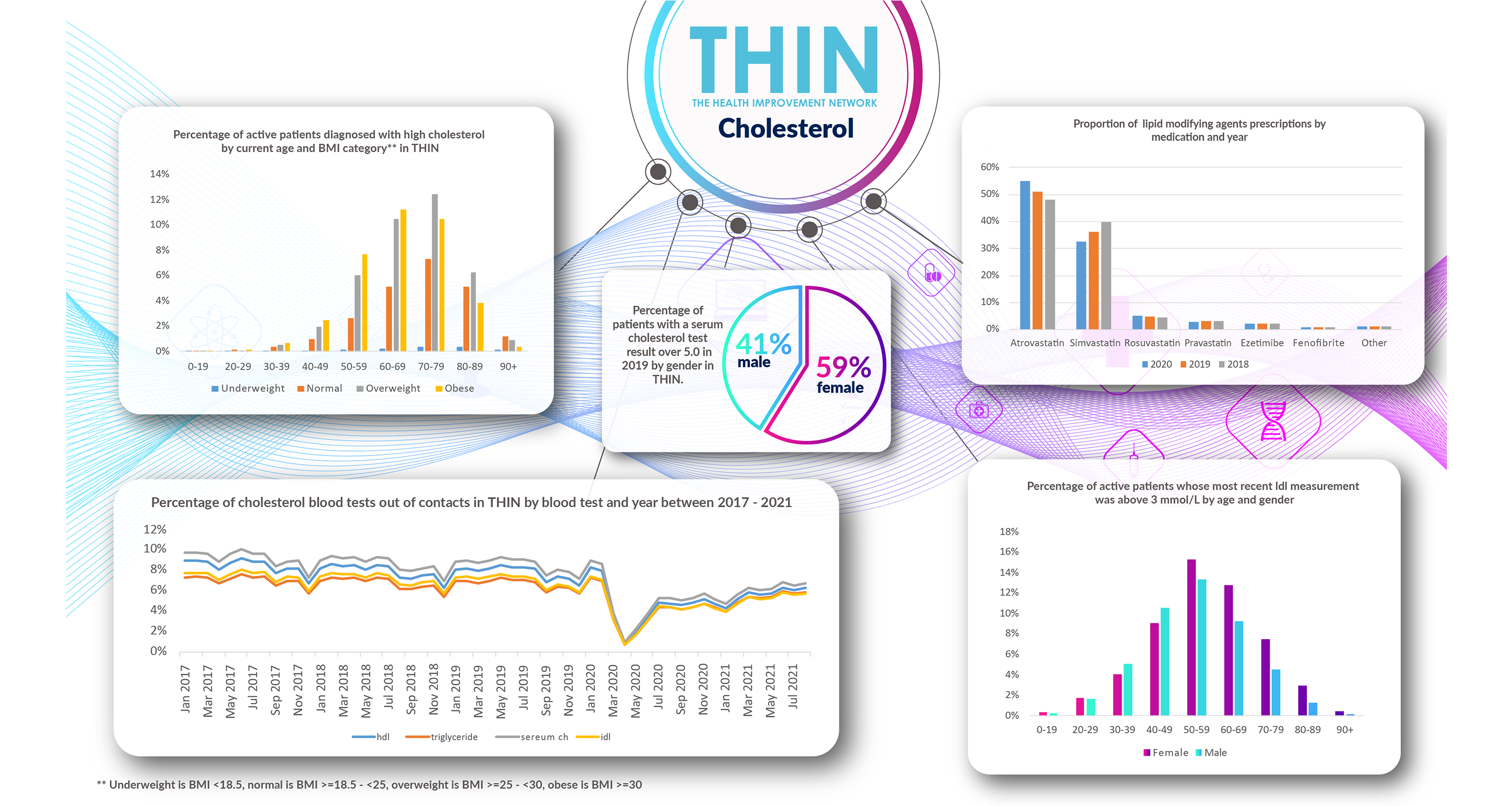
However, according to analysis of The Health Improvement Network (THIN®), a Cegedim database, analysis of the percentage of cholesterol blood tests out of contacts in THIN® by blood test and year between 2017 and 2021 confirms that tests plummeted in March 2020 and have yet to recover to pre-COVID 19 levels.
Which is one of the reasons why this October, during National Cholesterol Month, everyone is being advised to Talk about Cholesterol – and get a simple cholesterol test.
Understanding Cholesterol
Cholesterol is a soft, fat-like substance found in the body’s cells and helps form certain hormones and other necessary substances. Cholesterol tends to be classed ‘good’ (high density lipoprotein HDL) and ‘bad’ (low-density lipoprotein LDL).
Lifestyle plays a key role in raising levels, with risks including consumption of foods high in saturated fats, lack of exercise and physical activity, stress – with cortisol (the so-called stress hormone) increasing LDL-cholesterol, obesity and smoking.
Analysis of THIN® data confirms the link between weight and cholesterol - with a clear trend towards higher levels amongst the overweight and obese. For example: of those in the 50-59 age group, 82% of those with high cholesterol levels are overweight (35%) or obese (47%).
Identifying Risk
The only way to discover whether an individual is suffering from high cholesterol is a test because, in the majority of cases, there are no symptoms. The only exception is with familial hypercholesterolaemia (FH), which is associated with yellowish patches underneath the skin around the eyelids, white or grey discoloration of the peripheral cornea and xanthomata (deposition of yellowish cholesterol-rich material) of the tendons – and can be confirmed through genetic testing.
For the majority of the population, however, in the worst case scenario, a patient may only discover elevated levels as a result of heart attack, peripheral artery disease, or stroke due to atherosclerosis.
Regular Tests
Cholesterol tests can measure total cholesterol, including HDL and LDL, as well as triglycerides. Typically, healthy results are a totally cholesterol score of 5 or below. In more detail, clinicians are looking for, HDL I mmol/L or above; LDL 3 mmol/L or below, non-HDL 4 mmol/L or below; and triglycerides 2.3 mmol/L or below.
Over 4.3 million patients in THIN® have at least one HDL blood test record; around 5 million patients in THIN® have at least one serum cholesterol blood test record; and over 4.1 million patients in THIN® have at least one triglyceride blood test record. For around 16% of active patients in THIN the most recent LDL measurement was above 3 mmol/L.
Gender Difference
Analysis of THIN® also confirms the impact of menopause on women’s cholesterol levels. While high cholesterol is generally assumed to be more prevalent in men, there is a growing awareness that menopause can affect cholesterol levels. THIN® data confirms that women have lower cholesterol levels than men until they hit 50.
However, after the menopause females dominate the results: of active patients whose most recent LDL measurement was above 3 mmol/L, 54% of those aged 50-59 are women and by 60-69, 59% are female. Furthermore, 59% of active patients with a serum cholesterol test result over 5.0 in 2019 were female.
Managing Cholesterol
Taking a cholesterol test empowers individuals to take control and also ask for the right support. Sustained lifestyle changes including eat a well-balanced diet; limiting salt intake; exercising regularly; maintaining a recommended height-to-weight ratio and giving up smoking and alcohol can help individuals maintain healthy cholesterol.
In addition, the use of preventative treatments such as lipid modifying agents (known collective as Statins) has become standard practice over the past decade; indeed, Statins are the most prescribed drug in the UK, taken by an estimated eight million people.
Drug Adherence
However, concerns regarding side effects – which include muscle aches, fatigue, nausea and joint pain, are also known to affect patients’ drug adherence. Up to a fifth of people stop taking Statins, leading to both wasted medication and potential health implications. Yet according to a recent study, the side effects are not caused by the drug but by people believing it will make them unwell: the so called “nocebo effect” may account for 90% of the ill health associated with cholesterol lowering drugs.
Understanding the way patients respond to medication has become ever more important as the NHS looks to eradicate wastage and increase adherence. Analysis of THIN® reveals over 3.2 million prescriptions for lipid modifying agents were recorded in THIN® in 2020, with Atorvostatin (55%) and Simvastatin (33%) dominating prescriptions. It is interesting to note the rise in Atorvostatin prescriptions, up from 48% in 2018 and the reduction in Simvastatin, down from 40% in 2018.
Gathering Data
Given the large patient population now prescribed statins, there is a growing focus globally on assessing the potential wider impact on patient health beyond cardiovascular disease progression.
Most recently, results of a retrospective study linked statin use to diabetes progression; specifically, a greater likelihood of insulin treatment initiation, significant hyperglycaemia, acute glycaemic complications, and an increased number of prescriptions for glucose-lowering medication classes, researchers explained in JAMA Internal Medicine.
Overall, the results showed, “statin use was associated with a higher risk of diabetes treatment escalation and an increased risk of hyperglycaemic complications,” the authors concluded, a metabolic cost not considered in randomized controlled trials of statins. “Further research is needed to form a risk-tailored approach to balancing the cardiovascular benefits of statin therapy with its risk of diabetes progression.”
Given the ever rising numbers of patients diagnosed with type 2 diabetes such findings need to be taken into account by clinicians and patients – further reinforcing the value of population health data such as THIN® which provides invaluable insight into the overall health and wellbeing of patients within primary care.