Exploring Life Expectancy Equality during Men's Health Awareness Month
For decades, medical improvements and better living conditions have resulted in ever increasing life expectancy. Yet according to the Organisation Economic Cooperation and Development 2021 Health Indicators, life expectancy in Britain fell from 81.4 years in 2019 to 80.4 years in 2020, as a result of the high number of deaths caused by coronavirus. It is even more startling to consider therefore, that globally, men die on average five years earlier than women, and for reasons that are largely preventable.
According to Movember, a charity dedicated to changing the face of men’s health, there are three key contributors to this life expectancy divide: prostate cancer, testicular cancer and suicide. 10.8 million men globally facing life with a prostate cancer diagnosis – in the UK alone, Macmillan Cancer Support estimates around 500k men are currently living with prostate cancer. Globally, testicular cancer is the most common cancer among young men. And across the world, one man dies by suicide every minute of every day, with males accounting for 69% of all suicides.
Movember has a goal to reduce the number of men dying prematurely by 25% by 2030 - but how will the pandemic affect male life expectancy in both the immediate and long term? During Men’s Health Awareness Month this November it is vital to consider the impact Covid has had on this goal and consider the raft of issues that affect male life expectancy – from men’s health research to the way health services reach and support men.
Escalating Problem
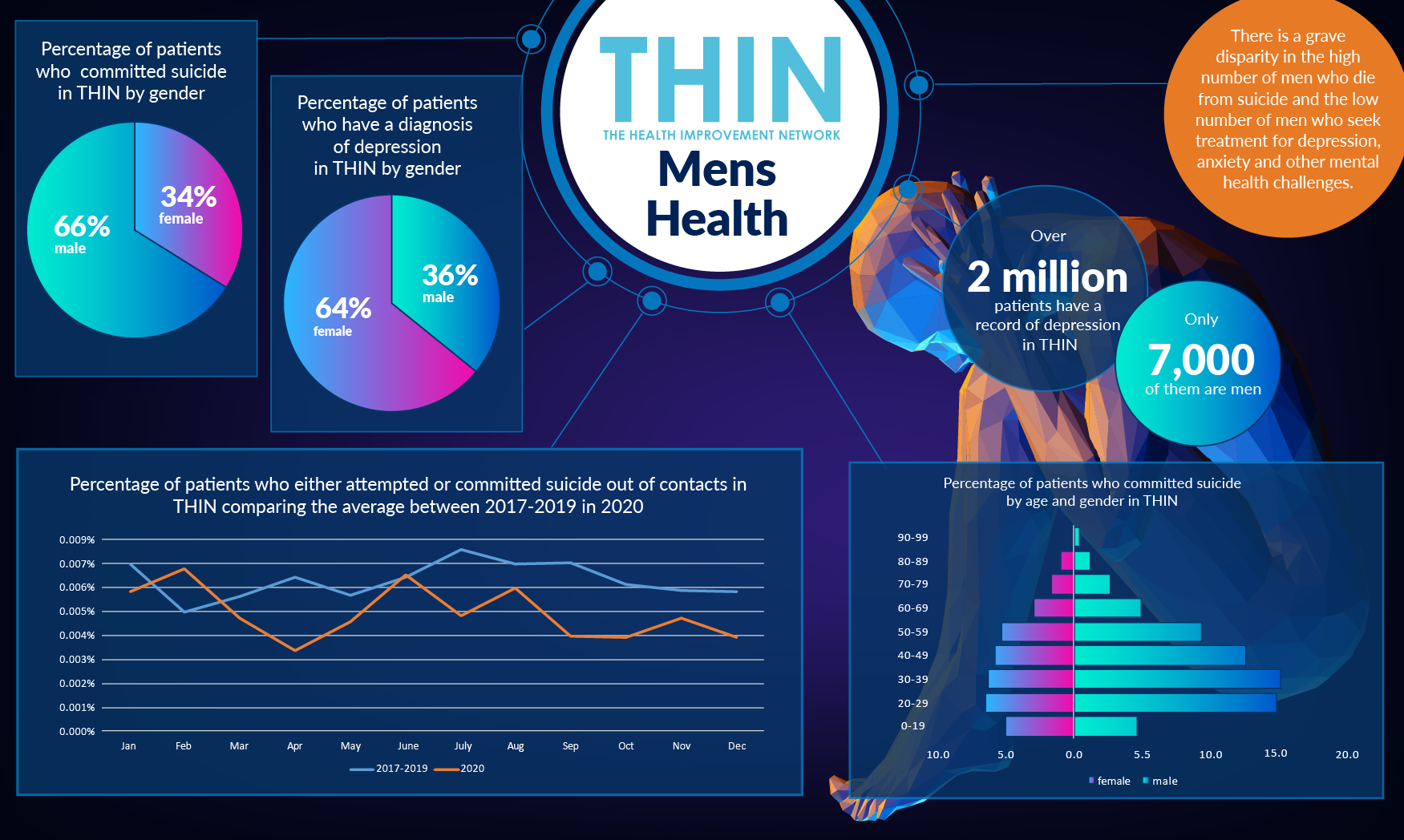
It is well documented that the pandemic has had a devastating effect on mental well- being, with cases of anxiety and depression around the world increasing dramatically in 2020. Researchers report an estimated 76m extra cases of anxiety and 53m extra cases of major depressive disorder than would have been expected had Covid not struck. While men appear to have been less severely affected than women, younger people of all genders have been heavily affected.
Following delays in cancer diagnoses at the beginning of the pandemic, cancer patients have been warned there is “worse to come” with Macmillan Cancer Support predicting a “perfect storm” due to the shortage of specialised cancer nurses in England and fears that the impact of the winter months and flu season could put further pressure on the NHS.
Delayed Diagnosis and Treatment
As with all cancers, early diagnosis is key to improving outcomes. However, one of the problems in diagnosing prostate cancer is that symptoms are rarely experienced until the tumour has grown large enough to put pressure on the urethra. There is currently no routine screening test for men in the UK – the standard prostate-specific antigen (PSA) testing remains controversial as it can lead to men being biopsied and treated unnecessarily, either because they don’t have cancer or have a type of cancer that would not cause harm.
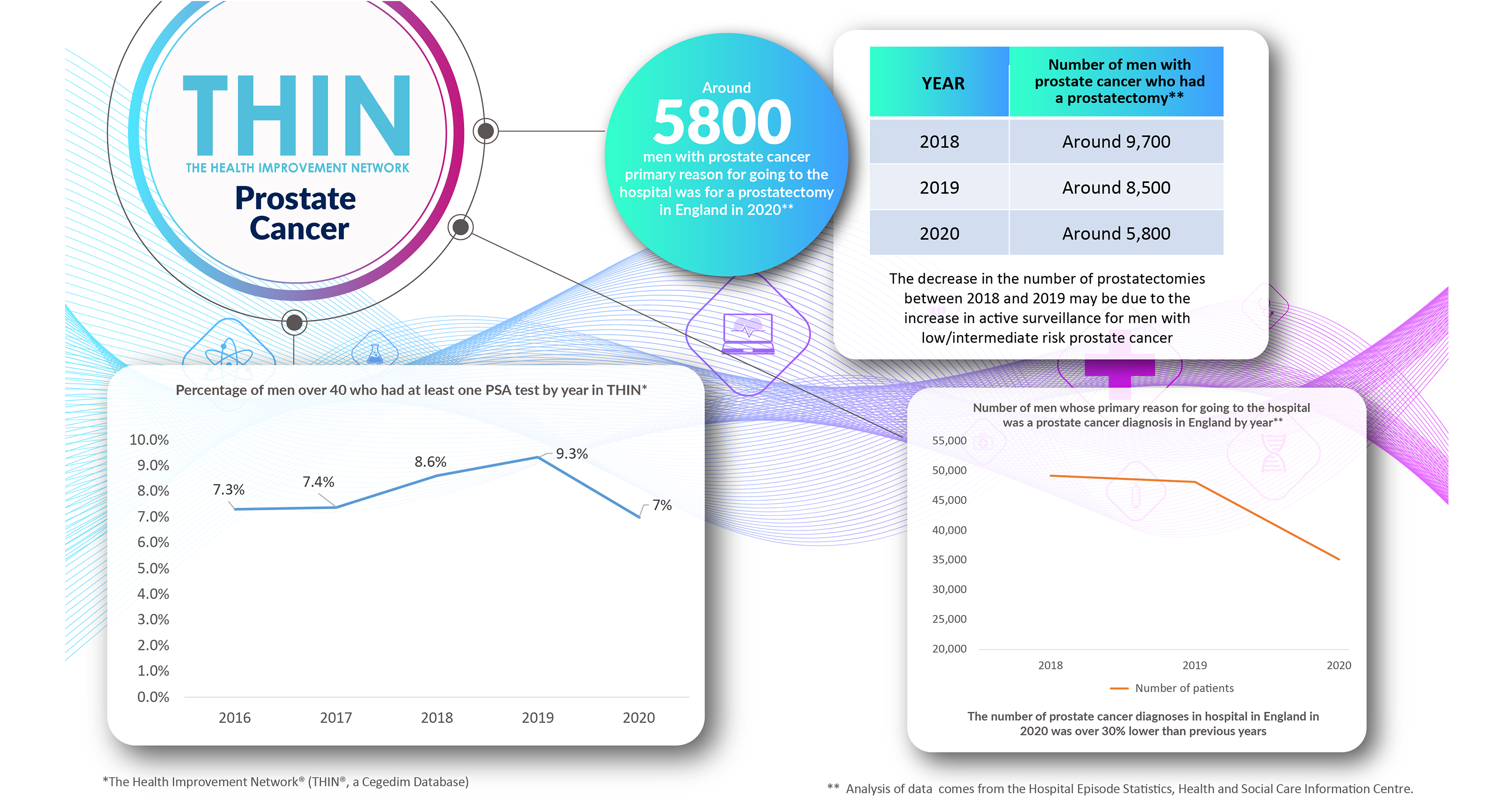
However, it is clear that the trends in diagnosis and treatment during the pandemic underline the very serious health implications for men with prostate cancer. According to analysis of The Health Improvement Network (THIN®), a Cegedim Database, testing for prostate cancer reduced during the pandemic – a reversal of the trend over previous years. While 9.3% of men over 40 had a least one PSA test per year in 2019, in 2020 that dropped to just 7%.
Furthermore, analysis of Hospital Episode Statistics from the Health and Social Care Information Centre, carried out by Cegedim Health Data UK, part of Cegedim Rx Limited, confirms the delays: the number of men for whom prostate cancer diagnosis was the primary reason for going to hospital was over 30% lower in 2020 than previous years. Treatment was also reduced– with prostatectomies reducing from 8,500 in 2019 to just 5,800 in 2020. While the treatment advice has in recent years prioritised active surveillance rather than surgery for men with low/intermediate risk prostate cancer, this reduction is over 30% - far in excess of the 12% drop seen in previous years.
Conclusion
What is the implication for long term health and life expectancy? According to the Prostate Cancer Charity, the numbers of men dying of prostate cancer continues to increase – rising to 12,000 men dying of prostate cancer in one year. Indeed, by 2030, prostate cancer will be the most common of all cancers - leading not only to death but also thousands of men experiencing treatment side effects that have a lasting impact on their body and well-being.
It has never been more important to get a true understanding of the overall picture of men’s health. Detailed analysis of population health will be key to understand the impact of the pandemic on male life expectancy. It will also provide both strategy makers and clinicians with the insight required to tailor services to meet men’s needs and better deliver the right patient care.